Introduction: Venous thromboembolism (VTE), defined as deep vein thrombosis (DVT), pulmonary embolism (PE), or both, represents a major cause of morbidity and mortality in patients with cancer. VTE is the second leading cause of death in patients with cancer, after cancer itself, in the United States. Previous studies have suggested differences by race in the occurrence of VTE among cancer patients. The purpose of this study was to investigate clinical differences in black and white patients with VTE and cancer.
Methods: We conducted an analysis of a CDC/Duke VTE surveillance project at the three hospitals in Durham County, North Carolina (Duke University Hospital, Duke Regional Hospital and the Durham VA Medical Center) from April 2012 through March 2014. A combination of electronic and manual review methods were used to identify unique Durham County residents with new diagnoses of objectively confirmed VTE. Data abstracted included demographics, risk factors including cancer, clinical data, treatment, and outcomes.
Results: A total of 1028 patients with a new VTE were identified during the surveillance period. Twenty-seven patients who were not black or white (e.g., race not listed; Asian; etc), and 41 with VTE affecting areas other than PE or limb DVT (e.g., cerebral sinus venous thrombosis) were excluded from this analysis. Of the remaining 960 patients, slightly more than half were female (497/960=51.8%), more than half were black (508/960=52.9%), almost a third were obese (337/960 = 35.1%), and median age was 59 years old. At the time of their VTE diagnosis, 184 patients with VTE (19.2%) had active cancer, defined as metastatic or diagnosed within the previous 6 months. The proportion of VTE associated with cancer varied by race. Among the 508 black patients with VTE, 111 (21.9%) had active cancer; in comparison, among the 452 white patients with VTE, 73 (16.1%) had active cancer (p-value=0.025).
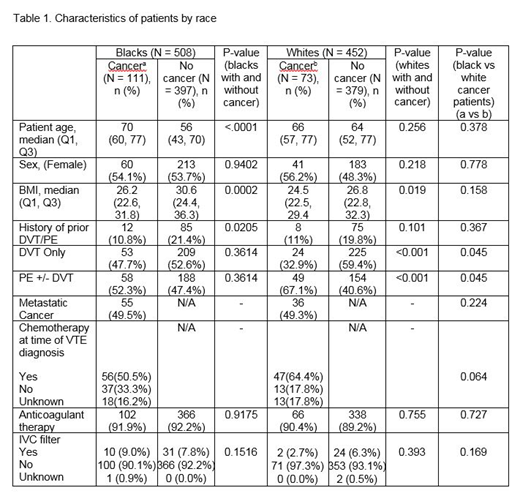
Black patients with VTE and cancer were older, had a lower body mass index (BMI), and were less likely to have sustained a prior VTE compared to black patients with VTE who did not have cancer (Table 1). Similarly, white patients with VTE and cancer had a lower BMI than white patients without cancer (Table 1). However, in contrast to the findings for black patients, white patients with VTE and cancer were not significantly older and did not show differences in having a prior VTE than white patients with VTE who did not have cancer. Additionally, white patients with VTE and cancer were much more likely to have sustained a PE, with or without DVT, and less likely to have sustained a DVT alone, than white patients with VTE who did not have cancer (Table 1). Black and white patients with both VTE and cancer, were similar in several aspects; however, white patients were less likely to have sustained a DVT alone and more likely to have sustained a PE, with or without DVT, compared to black patients.
The types of cancer most frequently encountered in black patients with VTE were gastrointestinal (24.3%), genitourinary (23.4%), and lung (18.9%), followed by breast (8.1%), gynecologic (9.0%) and hematologic malignancies (9.9%). The types of cancer most frequently encountered in white patients with VTE were lung (27.4%), breast (16.4%), and gastrointestinal (13.7%), followed by genitourinary (9.6%), gynecologic (8.2%) and hematologic malignancies (6.8%). Black and white patients with VTE and cancer were treated similarly to black and white patients with VTE who did not have cancer, with most receiving anticoagulant therapy and fewer than 10% receiving an IVC filter (Table 1). Enoxaparin was used most frequently, followed by warfarin.
Conclusions: There are several notable demographic and clinical differences between patients with VTE with and without cancer. While differences were observed for both black and white patients, several factors that were variable according to cancer status were unique to either black patients or white patients. One notable difference between black and white patients with both VTE and cancer was a lower proportion of DVT only and a higher proportion of PE, with or without DVT, in white patients.
Ortel:Instrumentation Laboratories: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal