Background: Thromboembolism (TE) is one of major causes of morbidity and mortality in patients with malignancy. Pathophysiological connection between TE and inflammation has been established and it is being thoroughly studied recently. The neutrophil to lymphocyte ratio (NLR) and the platelet to lymphocyte ratio (PLR) are biomarkers for systemic inflammation and might represent a yet unrecognized risk factor for development of venous thromboembolism in lymphoma patients having in mind chronic inflammatory milieu specific for lymphomas.
Aims: We aimed to investigate the association between NLR, PLR and future risk of TE, in a prospective cohort of lymphoma patients receiving chemotherapy.
Methods: We prospectively included 630 patients with B cell non Hodgkin lymphoma /indolent and agressive/, T cell non Hodgkin lymphoma and Hodgkin lymphoma who were diagnosed and treated (period 2014-2019.) at the Clinic for Hematology, Clinical Center of Serbia. Data for newly diagnosed patients, who had completed a minimum of one chemotherapy cycle, were collected for venous TE events from time of diagnosis to 3 months after the last cycle of therapy. NLR and PLR were calculated according to the CBC with differential count. TE complications were diagnosed based on clinical examination, laboratory evaluation and radiographic studies (duplex venous ultrasound, contrast-enhanced computed tomography scan, magnetic resonance imaging (MRI)). Response to therapy was assessed according to Cheson criteria. Logistic regression analysis and ROC curve were performed to assess the association of NLR and PLR with TE and therapy response. Cox regression and Kaplan Meier analysis were used to assess overall survival.
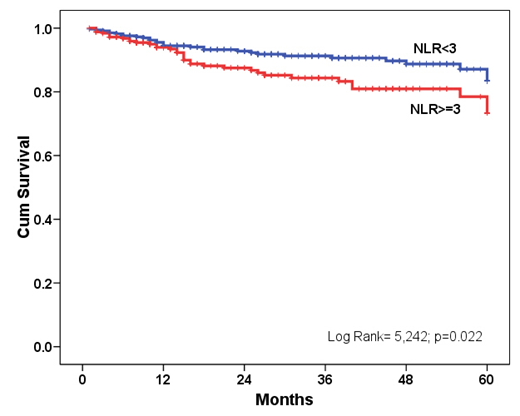
Results: The mean age in our group of patients was 53 years (range, 18-89 years) while 52.8% were males. Most patients had advanced stage disease: clinical stage III 20.6% and stage IV, 41.5%. A total of 327 patients (51.9%) had aggressive NHL; 175 (27.8%) had indolent NHL; 102 (16.2%) had HL; 26 (4.1%) had T cell NHL. 51 (8.2%) patients developed thromboembolic events. NLR and PLR were significantly higher in TE patients compared to patients without TE (p=0.001 and p=0.002, respectively). The NLR was positively associated with PLR (p<0.001). A positive NLR was considered 3 or higher, while a positive PLR was a ratio of 10 or more. The ROC curve analysis demonstrated acceptable specificity and sensitivity of NLR and PLR in predicting TE. NLR and PLR were found to be prognostic factors for the TE (relative risk [RR] = 2.9, 95% confidence interval [CI] = 1.6-5.3, p=0.001 and RR=2.7, 95% CI =1.4-5.1, p=0.002, respectively) as well as for overall response to therapy (RR=2.7, 95%CI=1.7-5.7, p<0.001 and RR=2.0, 95%CI=1.1-3.4, p=0.015, respectively). Regarding the overall survival, in univariate analysis there was an association of the development of TE and decreased survival, while in multivariate model NLR was found to be an independent risk factor for overall survival in lymphoma patients (HR=1.8, 95%CI=1.1-2.9, p=0.024) (Figure 1).
Summary/Conclusion: NLR could represent useful clinical predictor of TE complications in patients with lymphoma without additional costs to the national health systems. Our research showed that NLR is also predictive for response to therapy and overall survival of lymphoma patients. Simplicity, cost effectiveness, and rapid turn around qualify this new tool for routine prognostic assessment in lymphoma patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal