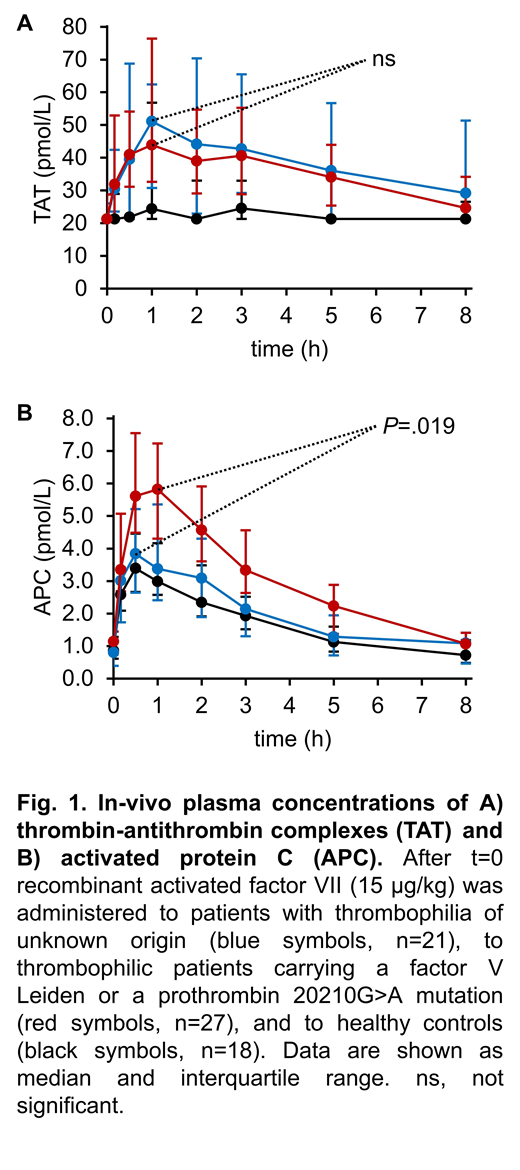
Background: In a large proportion of patients with unprovoked venous thromboembolism (VTE), no risk factors can be identified. Recently, we have shown that an increased activated protein C (APC) response to in vivo thrombin formation reduces the thrombotic risk of factor V Leiden (FVL) carriers but not of prothrombin G20210A mutation (PTM) carriers. In vivo thrombin formation was triggered by low-dose administration of recombinant activated factor VII (rFVIIa) followed by hemostasis biomarker monitoring. Aim of the present study was to extend this SHAPE approach to patients with thrombophilia of unknown origin. Methods: The study population consisted of 21 subjects with a positive self-history of unprovoked VTE (VTE+) as well as a positive family history, in whom no established thrombophilic risk factor was detectable (thrombophilia of unknown origin, TUO). A second cohort included 27 VTE+ patients tested positive for FVL (n=14) or PTM (n=13). None of the subjects was under anticoagulant treatment at the time of analysis. The control group consisted of 18 healthy volunteers. Blood samples were collected immediately before and during a period of 8 hours following injection of 15 µg/kg rFVIIa. Plasma levels of free thrombin and APC were quantified using oligonucleotide-based enzyme capture assays (OECAs). Prothrombin activation fragment 1+2 (F1+2), thrombin-antithrombin complex (TAT), and D-dimer were measured additionally. Results: Injections of rFVIIa were well-tolerated by all subjects and median D-dimer levels remained within the reference range in all three cohorts. Plasma levels of F1+2 increased after rFVIIa injection, showing no significant differences between the groups. A comparable increase of TAT was observed in both TUO patients and VTE+ mutation carriers, from a median of 21.3 to 51.1 pmol/L (P=.022), and from 21.3 to 43.9 pmol/L, respectively (Figure 1A). Median levels of TAT in the controls and median levels of free thrombin in all cohorts remained below their respective quantifiable limits after rFVIIa injection. APC increased from 0.80 to 3.84 pmol/L (P=.001) in TUO patients, from 1.14 to 5.82 pmol/L (P<10-4) in VTE+ mutation carriers, and from 0.87 to 3.39 pmol/L (P=.001) in the control group. The APC increase was significantly smaller in the TUO cohort than in the VTE+ mutation carriers (P=.019) (Figure 1B). Conclusion: A low APC response to an increased in vivo thrombin formation is a frequent finding among patients with thrombophilia of unknown origin. This finding is in line with previous data suggesting that higher APC levels protect FVL carriers from thrombosis development. The results of the present study further suggest that a low APC response might be an independent risk factor of VTE. Further studies are warranted to identify the factors that modulate the APC response.
Rühl:Sanofi Genzyme: Honoraria; SOBI: Honoraria; Shire: Honoraria; Bayer: Honoraria; CSL Behring: Honoraria; Grifols: Honoraria. Reda:Shire: Honoraria; Grifols: Honoraria. Winterhagen:SOBI: Honoraria. Berens:Pfizer: Honoraria; Shire: Honoraria; Biotest: Honoraria; CSL Behring: Honoraria; NovoNordisk: Honoraria; Baxter: Honoraria. Müller:Roche: Membership on an entity's Board of Directors or advisory committees; Siemens: Membership on an entity's Board of Directors or advisory committees; Bayer: Membership on an entity's Board of Directors or advisory committees; NovoNordisk: Membership on an entity's Board of Directors or advisory committees. Oldenburg:Grifols: Consultancy, Speakers Bureau; Roche: Consultancy, Speakers Bureau; Bayer: Consultancy, Research Funding, Speakers Bureau; Swedish Orphan Biovitrum: Consultancy, Speakers Bureau; NovoNordisk: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Speakers Bureau; Octapharma: Consultancy, Research Funding, Speakers Bureau; Biotest: Consultancy, Research Funding, Speakers Bureau; Chugai: Consultancy, Speakers Bureau; CSL Behring: Consultancy, Research Funding, Speakers Bureau; Takeda (Shire): Consultancy, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal