Introduction:
Immune checkpoint inhibitors (ICI) have proven to be a significant breakthrough in modern cancer therapy. However, this has come at a cost of immune-related adverse events (irAE) affecting various organ systems. Hematological irAEs including autoimmune hemolytic anemia (AIHA), pure red cell aplasia (PRCA), immune thrombocytopenia (ITP), thrombotic thrombocytopenic purpura (TTP), hemophagocytic lymphohistiocytosis (HLH), aplastic anemia and pancytopenia, are well recognized side effects of ICI. Due to their rarity, existing literature is confined to case reports and series. We conducted a systematic review of all published case reports and series till date to summarize clinical presentation, risk factors, management, and outcomes of patients who develop hematologic irAEs during ICI treatment.
Methods:
Using free text and controlled vocabulary (MESH and EMTREE terms), we performed a systematic search of the literature using Ovid Embase, Ovid Medline, Pubmed, Scopus, and Web of Science Core Collection. Eligibility criteria included any case report or case series describing at least one hematologic irAEs developing during and likely related to ICI therapy for solid/hematologic malignancy. Two authors independently screened the titles, abstracts, and the full text of the selected papers. Patients who had received at least one FDA approved ICI (PD-1, PDL-1 or CTLA-4 inhibitors), and subsequently developed a decline in one or more of cell lines were included. Data regarding clinical presentation, concomitant other irAEs, treatment and clinical outcomes was extracted using a standardized data extraction form and summarized using descriptive statistics.
Results:
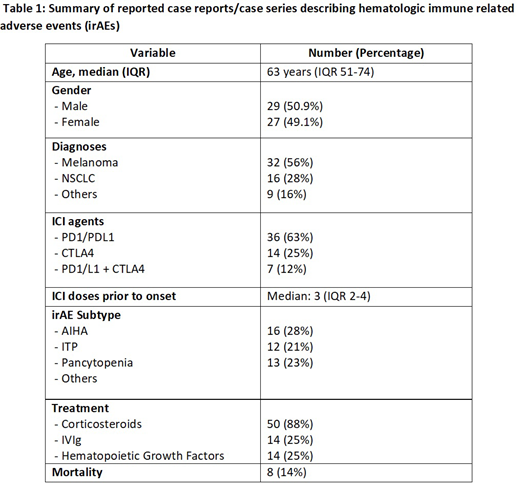
Of the 19856 articles screened, a total of 59 articles were selected for full-text review, and a total of 54 reports describing 57 cases met our eligibility criteria. The median age at the time of presentation was 63 y(interquartile range (IQR) 51-74) yrs, and 29 (50.9%) were males. PD-1 inhibitors were implicated in 35 (61%), CTLA-4 inhibitors in 14 (25%) and PD1/CTLA4 combination therapy in 7 (12%). The most common malignancies included metastatic melanoma (n=32, 56%) and non-small cell lung cancer (n=16, 28%). Only 8 patients (14%) reported a pre-existing history of autoimmune disease and only 11 (19%) had additional irAES involving other organ systems.
AIHA (n=16, 28%), ITP (n=12, 21%) and pancytopenia (n=13, 23%) were the three most common subtypes of hematologic irAEs. Two or more cell lines were affected in 13 patients (23%). Twenty-six (46%) of the irAEs were detected on regular laboratory tests. The median number of cycles prior to the onset of hematologic irAEs was 3 (IQR 2-4). Among treatment strategies, corticosteroids were used in most patients (n=50, 88%). Other treatment modalities employed included Intravenous Immunoglobulin (IVIg) (n=14; 25%), hematopoietic growth factors and other supportive treatment were Treatment strategies were based on the actual irAE and the patient's condition. Corticosteroids, transfusion of blood products, hematopoietic growth factors, and other supportive treatment were primarily employed in most patients. Steroids were used in 50 (88%) patients and intravenous immunoglobulins in 14 (25%). Other immunosuppressants, anti-thymocyte globulins, and plasma exchange were used in select patients. Most of the patients (n=44, 77%) were described as having improved or recovered blood counts with treatment. Only 5 (9%) of these patients were rechallenged with the same or other ICI therapy. Among these, the same hematologic irAE recurred in 2 patients (40%). Cytopenia, as an irAE, was directly responsible for the death of 8 patients (14%).
Conclusion:
Hematologic irAEs are rare but potentially fatal adverse effect of ICI therapy. Although it can have diverse manifestations, AIHA and ITP are the most common subtypes. Almost half of these patients are clinically silent and detected in routine laboratory evaluation. Most hematologic irAEs appear early during the course of therapy and without pre-existing/concomitant irAEs. Most cases report successful resolution with treatment that commonly include high dose corticosteroids, and successful re-challenge has been reported in a few cases.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal