Background Autoimmune neutropenia is a chronic reduction of absolute neutrophil below the threshold for age, due to peripheral destruction by specific antibodies (AaN). "Primary autoimmune neutropenia" (pAN) usually appears in early infancy and generally resolve within 18-24 months, while "Secondary autoimmune Neutropenia" (sAN) rises later in life and is usually accompanied by autoimmune features. Very few descriptions on the topic are available in the literature. Aim of the study: to describe from a clinical and immunological point of view a cohort of subjects affected with sAN included registered in the Italian Neutropenia Registry (INR) and to compare these data with those from subjects diagnosed with pAN still in the INR .
Patient and methods Subjects with neutropenia and positivity of AaN lasting for more than 2 years in subjects older than 5 years of life ( up to 18) or patients affected with neutropenia (plus AaN) associated with autoimmune features registered in the INR from 2005 to 2018 were considered eligible for the present study. Antibodies against neutrophils were always detected throught indirect test .
Results: Data from 40 patients affected with sAN (26 females, 65%) were collected. Median age at diagnosis was of 11.6 years (0-21.558mo) with a median follow up of 17 months (0-159mo). The degree of Neutropenia was mild in 12.5%(5/40), moderate in 35% (14/40) and severe in 52.5% (21/40) Neutropenia was diagnosed by chance in half of the cohort and in only 10% (4/40) (10%) definitively resolved . Neutropenia coexisted with leucopenia in almost all the of subjects (36/40, 88%), and moreover, autoimmune haemolytic anemia and thrombocytopenia was concomitant to neutropenia in 12% (5/40) and 32.5% in (13/40) of cases respectively.
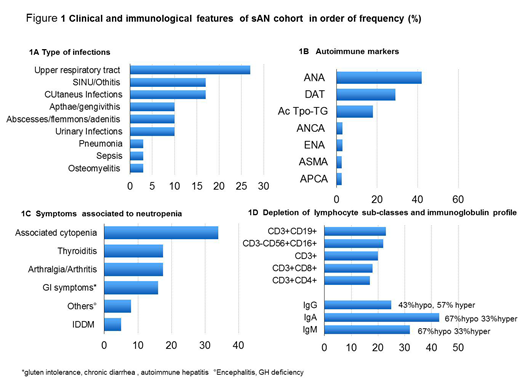
As for clinical history, 15% (6/40) subjects (15%) were completely asymptomatic , while the remaining 85% (36/40) (85%) had clinical signs of infections and/or autoimmunity features . Infections were documented in 60% (24/40) (60%) of patients. Severe infections namely sepsis , meningitis, pneumonia, osteomyielitis and broad absesses/flemmons were identified in 21% (5/24) of the group. Other type of infections are listed Figure 1A. Apparently there was no correlation between severity of infections and degree of neutropenia ( p=0.2 Fisher' exact test) Autoimmune features and/or autoimmunity markers were present in 30/40 (75% ) of the entire cohort . Thyroiditis and artralgia/arthritis were the most common signs which accounted both for 17,5% of the total episodes. Positivity of ANA and Direct antibodies test ( DAT) were showed in 42% and 29% of cases respectively. (Fig 1B, 1C)
As for immunological characteristic 37% (12/32) of the studied subjects were frankly lymphocytopenic, 19% (6/32) had borderline values , while the remaining 44% (14/32) had normal lymphocytes subclasses. In terms of frequency of sub-classes depletion CD19 + and NK were the most frequently decreased subsets. ( Fig 1D) . Dosage of serum immunoglobulin (IgG, IgM and IgA) were shown for all three classes were abnormal (either increased or diminished) in 74% (28/38) of patients (Fig 1D).
Mutation analysis performed by Next Generation Sequencing in 16/40 subjects and pathogenic variants of : TACI, TINF 2, CASP 8, CASP 10, PI3K, CARD 11 genes were identified in 4/16 (25%).
As for treatment, in 25 % of cases needed Granulocyte-Colony Stimulating Factor to control infections. Rapamicin, micophenolate mofetil, steroids, intravenous immunoglobulin were necessary in 25% (10/40) of patients cases, being (4 of them were already treated on with G-CSF)
Comparison with a group of 236 pAN patients of the INR showed that sAN were older at diagnosis (P<0.0001), had far inferior rate of resolution (P<0,0001), were more frequently leucopenic (p<0,0001), more rarely with monocitosis (p=0.015), had more frequently CD19 and NK depletion (p<0.00019), associated cytopenia and autoimmune symptoms and markers ( p<0.0001) while infection burden were slightly increased but not significantly different compared with pAN( p=0.2).
Conclusions This registry study describes the clinical phenotype of sAN appearing in childhood and by comparative analysis shows that sAN substantially differs from pAN. sAN indeed appears an epiphenomenon of a complex immunological disturbances rather than a disease itself. Occasionally mutations of genes of immunodeficiency/disimmunity can be demonstrated
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal