Background: ENDARITM (oral pharmaceutical L-glutamine powder) received FDA approval in 2017 as a treatment for sickle cell disease (SCD). A pivotal phase 3 clinical study conducted by Emmaus Medical, Inc. showed that L-glutamine resulted in a lower incidence of vaso-occlusive crises (VOC) as well as a lower rate of hospitalizations and shorter hospital stays. No changes in standard clinical laboratory values were noted. The clinical improvements associated with sickle cell complications are believed to be due to an increase in the proportion of the reduced form of nicotinamide adenine dinucleotides in the red blood cells (RBC) of patients with SCD, reducing the oxidative stress. While the endpoints in the phase 3 study are clinically important, it is essential that we identify biomarkers or measurable laboratory changes that can serve as endpoints for future clinical trials assessing dose optimization and the efficacy and safety of L-glutamine in SCD individuals, including those with hepatic and renal dysfunction. RBC rheology is markedly abnormal in SCD; blood is more viscous for a given hematocrit than normal individuals, dense red blood cells (DRBC) are packed with HbS, potentiating sickling, and RBCs are less deformable than those of HbAA or HbAS individuals. High whole blood viscosity, high DRBCs, and poor RBC deformability are associated with higher rates of VOC. Given the demonstrated reduction in pain events, we hypothesized that L-glutamine might improve RBC rheology and sought to test this in vitro and in vivo using a battery of rheological tests.
Methods: For the in vitro study, 6 mL of whole blood was drawn into an EDTA vacutainer from ten pediatric patients with sickle cell anemia (HbSS or HbSβ0) during routine clinical checkups under an IRB approved protocol. The cohort included 3 female and 7 male patients, ages 2-19 years old. All patients were on a steady dose of hydroxyurea and did not receive a transfusion within the 3 months prior to sample collection. A 200 mM stock solution of L-glutamine and water was mixed and filtered under light-protected conditions. Aliquots were stored at -20°C to avoid multiple freeze/thaw cycles. L-glutamine was added to 3 mL of whole blood for a final concentration of 1 mM (average in vivo L-glutamine plasma concentration in patients with SCD treated with L-glutamine); 3 mL of the same patient sample with water added served as a control. After a 24-hour incubation period at 4°C, whole blood viscosity was measured using a cone and plate viscometer at 37°C (DV3T Rheometer, AMETEK Brookfield, USA), %DRBCs were measured on an ADVIA 120 Hematology System (Siemens Healthcare Diagnostics, Inc., USA), and deformability measured using a Laser Optical Rotational Red Cell Analyzer (Lorrca®) (RR Mechatronics, the Netherlands) with the Oxygenscan module. The Oxygenscan measures RBC deformability at normoxia (Elmax), deformability upon deoxygenation (EImin), and point of sickling (PoS), the oxygen tension at which deformability begins to decline, reflecting the patient-specific pO2 at which sickling begins. Paired samples (with and without added L-glutamine) were analyzed using Student's t-test. For the in vivo study, rheological tests were performed on peripheral blood from one patient (18-year-old male on hydroxyurea) at baseline and treated with L-glutamine as part of his routine clinical care.
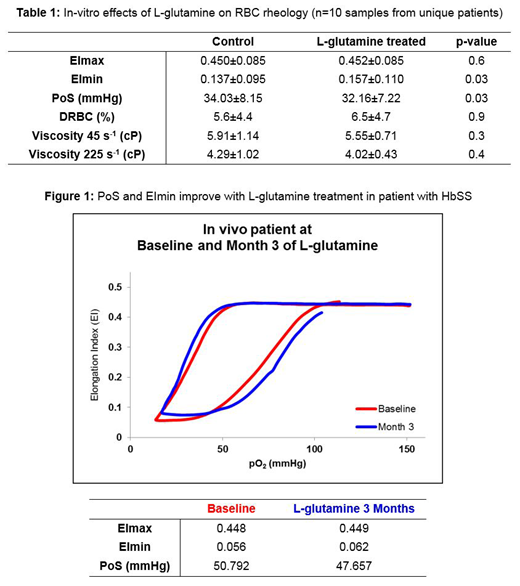
Results and conclusions: Addition of L-glutamine in vitro significantly reduced the PoS, meaning RBCs incubated with L-glutamine could tolerate a lower pO2 before sickling compared to the control. RBCs incubated with L-glutamine also had significantly higher EImin, meaning deoxygenated RBCs were more flexible and deformable. Whole blood viscosity at 45s-1 and 225s-1 did not change significantly following incubation with L-glutamine; %DRBCs also did not change significantly (Table 1). The in vivo patient sample tested exhibited a similar improvement in PoS and EImin (Figure 1). We therefore propose to further test the performance of the PoS and EImin as possible biomarkers of response to L-glutamine in vivo. If validated, these biomarkers may also help further elucidate the mechanisms of action of L-glutamine in SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal