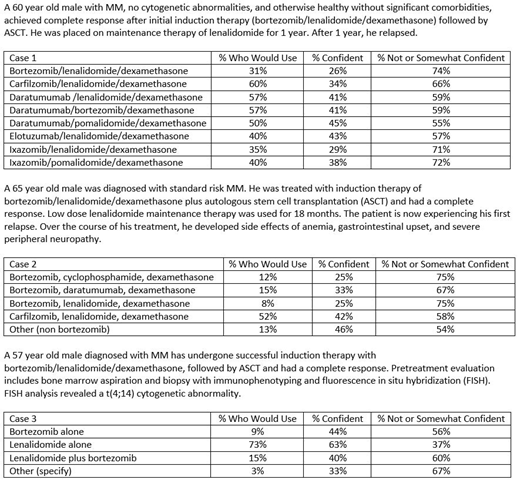
Introduction: Two surveys were conducted to understand the rationale for hematologists/oncologists (hem/oncs) to seek continuing medical education (CME) as well as how the information is applied to clinical practice. Additionally, we studied the clinical decision making of hem/oncs who treat patients with multiple myeloma (MM) in order to understand the areas to focus for future CME activities. Methods: We conducted two incentivized surveys where only hem/oncs in the US who treat patients were eligible: 1) MM decision-making survey (MM survey) in November 2018 where they were asked case-based questions to assess practice patterns and they were asked to rate their level of confidence in their decisions for the cases; and 2) Information seeking behaviors and preferences survey (behavior survey) in May and June 2019 where they responded to questions about what information informs practice and how often they need new information. Physicians were paid for their participation in the surveys. Results: 93 hem/oncs participated in the behavior survey with 56% from the community setting and 44% practicing exclusively in an academic setting. Community hem/oncs visit online CME more frequently than academic hem/oncs (daily or at least once a week: 67 vs 51%, respectively). The primary factors driving hem/oncs to access online CME include the need to learn about the latest developments (45%) and looking for an answer to a specific question (25%). Community hem/oncs are 2x more likely than academic hem/oncs to access online CME in order to earn credits. All of the hem/oncs surveyed have modified or implemented a new clinical practice in the last year, with the majority of the modified or new practices related to treatment (69%). Community hem/oncs are 174% more likely than academic hem/oncs to use CME as the source of the information leading to modified/new practice (27% vs 10%). The influence of CME on clinical practices is especially striking among hem/oncs practicing in a community vs academic setting on both gaining more confidence in their current practices (71% vs 59%) and modifying treatment practices (64% vs 54%). There were 101 hem/oncs who participated in the MM survey with 51% practicing in the community setting and 55% seeing between 1 to 10 patients with MM per month, whereas 22% saw more than 20 patients with MM per month. Case 1 highlights the lack of confidence among hem/oncs in making treatment decisions for patients with relapsed/refractory MM, with the majority, between 55% to 72%, only somewhat or not confident in their clinical decision. Although various options would be acceptable and not harmful, ideally treatment decisions would be made with a sense of confidence. In case 2, a striking 48% of hem/oncs would use a bortezomib-based regimen in a patient who has severe peripheral neuropathy, despite bortezomib's known side effect of peripheral neuropathy. For those who would use carfilzomib (52%) or a non-bortezomib regimen (13%), less than half (42% and 46%, respectively) were confident in their decision. Case 3 highlights the complexity of tailoring therapy for patients with MM as any of the answers could be appropriate, but between 37% and 67% of hem/oncs were only somewhat or not confident in their choices, indicating a need for additional education. Conclusions: Large Impact of CME on Community Hem/Oncs: A majority of hem/oncs access online CME at least once a week in order to learn about the latest developments and to find answers to specific questions, with the need for CME credits being a minor driver of CME consumption. The data show that CME has a high impact on clinical practices as the majority of hem/oncs surveyed modified or implemented new clinical practices in the last year as a result of what was learned in CME activities. The impact of CME on clinical practices is particularly striking among hem/oncs who practice in community-based settings. Additional Multiple Myeloma-Focused CME is Needed:The treatment paradigm for MM is rapidly evolving and this analysis shows that in order to improve the skills of hem/oncs as well as their confidence in their clinical decision making, additional CME is needed in the areas of (1) individualizing treatment for R/R MM, (2) managing adverse events, and (3) selecting maintenance therapy for high-risk MM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal