Introduction
South Africa has a high prevalence of Human immunodeficiency virus (HIV) infection with an estimated 7 million people with HIV (PWH). Significant progress has been made in implementing anti-retroviral therapy (ART) with 4 million patients on ART in 2017 compared with 400 000 in 2007. HIV-associated lymphomas remain a public health concern in our setting. Patterns of changes in lymphoma are well documented in high-income countries following wide-scale ART, however, there are limited published data available from our region. This study aimed to compare epidemiological characteristics of high-grade B-cell lymphomas (HG BLPDs) in PWH presenting to the academic hospitals in Johannesburg, South Africa, prior to and post implementation of a wide-scale ART programme.
Methods
This study was approved by the Human Research Ethics committee of the University of the Witwatersrand (protocol number: M130280). All patients with newly diagnosed lymphoma (B- and T-cell non-Hodgkin and Hodgkin lymphoma) during 2007 and 2017 in the Johannesburg academic complex of hospitals (South Africa) were identified via a comprehensive search of the laboratory information system (LIS) utilizing SNOMED codes and a detailed pathology record review. Limited demographic and clinical data were collected for each patient. Statistical analysis was performed using GraphPad Prism software, version 7.0 (San Diego, California, United States). Continuous data are presented as the median (interquartile range (IQR)) and categorical data as frequencies and percentages. The Mann-Whitney and Fisher's exact or Chi-square test were used to compare continuous and categorical variables respectively.
Results and Discussion
The total number of cases of lymphoma diagnosed in the Johannesburg state-sector hospitals showed a marked increase from 397 in 2007 to 582 in 2017. This may represent an improvement in access to health-care, more extensive diagnostic work-up and significantly increased HIV testing in lymphoma patients (p<0.0001) in the later time period. HG BLPDs remained the most commonly diagnosed lymphoma subtype, comprising 69% (2007) and 60% (2017) of all lymphomas diagnosed and 78% and 69% of cases in PWH with lymphoma respectively.
There were significantly more PWH presenting with HG BLPD on ART in 2017 (p<0.0001), with a median duration of therapy of 24 months (interquartile range 12-48). No significant change in the percentage of patients with extranodal (68.4% vs 73.1%) or bone marrow involvement (26.9% vs 24.2%) was noted. There was no significant change in prognostic markers, with the exception of lactate dehydrogenase (LDH) levels which showed a significant decline in 2017 (p<0.0001). This may be due to a significantly increased absolute number and proportion of diffuse large B-Cell Lymphoma (DLBCL) cases relative to the other HG BLPDs which were diagnosed in 2017 (p=0.0004), whilst Burkitt leukemia/lymphoma (BL) and high-grade B-cell lymphoma (HGBL) showed no significant increase (p=0,1886), and plasmablastic lymphoma (PBL) appeared to have declined in overall number and proportion (although this did not reach statistical significance (p=0,0721)).
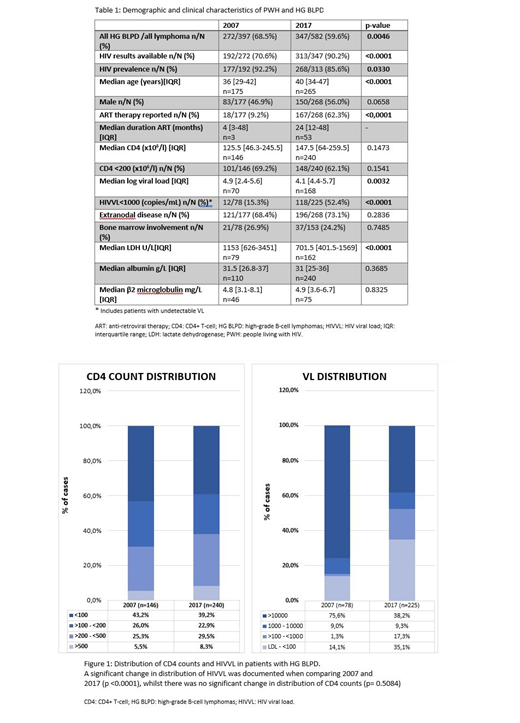
PWH presenting with lymphoma showed significant changes in virologic control as expected, with a significant decline in the median HIV viral load (HIVVL) (p=0.0032), increase in the proportion of patients with an HIVVL <1000 (15.3% in 2007 vs 52.4% in 2017; p<0.0001) and changed distribution of VL (p<0.0001) in 2017 as compared to 2007 (Table 1 and Figure 1). Despite the improvement in virological suppression, there was no significant change in median CD4+ T-cell count (p=0.1473), change in proportion of patients with CD4 count<200 x106/l (69.2% in 2007 vs 62.1% in 2017; p=0.1541) or change in distribution of CD4 counts (p=0.5084) (Table 1 and Figure 1).
Conclusions:
A marked increase in the number of lymphoma cases diagnosed in the state-sector hospitals in Johannesburg was noted over the study period with HG BLPD remaining the most commonly diagnosed subtype in PWH despite significant improvements in virological control. This suggests that virological control alone may not be protective and that delayed or incomplete immunologic recovery as a consequence of late ART initiation may be contributing. Public health initiatives to promote early access to ARV therapy at higher CD4 counts may assist in decreasing the incidence of HG BLPDs in our setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal