Background:
Non-Hispanic Black (NHB) and Hispanic patients with Acute Myeloid Leukemia (AML) have higher mortality rates than non-Hispanic white (NHW) patients despite a lower incidence of disease, more favorable genetics and younger age at presentation (Patel. AJCO 2015). It is unknown whether these disparities are linked to disease biology or treatment approach. Prior large database analyses have suggested that differences in AML outcomes may be impacted by socioeconomic factors such as insurance status and household income but lack data regarding treatment details including complications and molecular disease features (Bhatt. Blood Advances 2018). We postulate that increased mortality rates for NHB and Hispanic patients with AML are driven by disparities in treatment patterns when adjusted for baseline disease risk.
Methods:
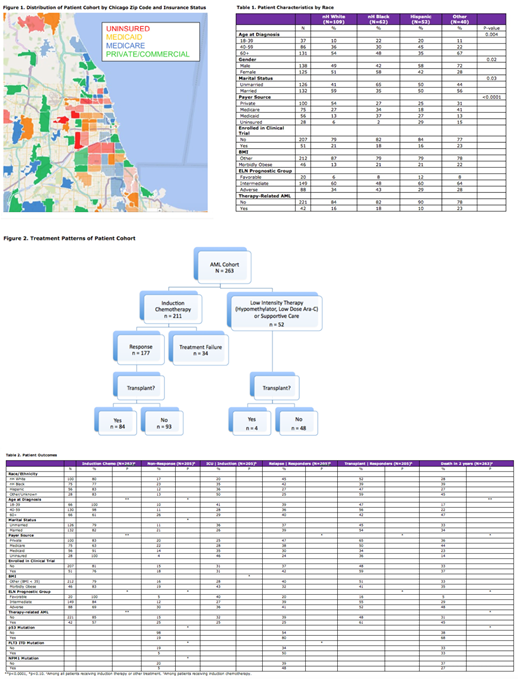
We have analyzed data collected on consecutive adult patients diagnosed with AML between 2012 and 2018 from 5 academic cancer centers in Chicago surveying different population subsets using an IRB approved protocol. Figure 1 shows insurance status of the patient cohort by zip code. Cox proportional hazards models will be used to estimate multivariable-adjusted hazard ratios for relapse and mortality. Baseline models will be adjusted for age, gender and race/ethnicity to estimate the hazard ratios for the NHB-NHW and Hispanic-NHW disparities in time to relapse and treatment-related or disease-related mortality.
Results:
At the time of abstract submission 263 subjects were included in the analysis. The study is actively accruing at all 5 institutions with a database goal of 700 patients. There are significant differences in baseline characteristics by race/ethnicity (Table 1). NHB patients are younger, less likely to be married, and less likely to be privately insured than NHW (20% vs >51%). Hispanic patients are younger and more likely to be uninsured than NHW patients (30% vs 6%), likely reflective of County Hospital patients. In this preliminary dataset, clinical trial enrollment rates were similar by race/ethnicity. The distribution of ELN risk groups (Dohner. Blood 2017) and therapy-related AML (t-AML) cases were also similar by race/ethnicity.
Eighty percent of patients received intensive induction chemotherapy (Fig 2). Receipt of intensive therapy did not differ by race but was more prevalent in younger patients and uninsured patients (Table 2), likely related to concerns about outpatient medication coverage. Elderly, adverse ELN risk and t-AML patients were less likely to receive intensive chemotherapy, likely due to poorer performance status in the elderly and potential chemo-resistance in p53mut AML.
Treatment complications during induction chemotherapy, as captured by ICU admissions, were significantly lower in NHW patients, and significantly increased in morbidly obese patients.
Treatment failure, by IWG criteria, did not differ by race but rather was determined by disease specific factors including ELN group, and t-AML. Relapse risk was higher in FLT3-ITD mutant cases. Allogeneic transplant rates did not differ significantly by race but were higher in adverse ELN groups and in privately insured patients. Two-year survival was affected by individual and disease specific factors including age, Medicare enrollment, t-AML and ELN risk group.
Discussion:
Our current dataset (n = 263) highlights disparities in treatment approaches in patients with AML. These include i) the preferential utilization of intensive induction chemotherapy in younger patients and those lacking high risk molecular features, and ii), the influence of payer status and molecular risk on utilization of allogeneic stem cell transplant in first remission. Treatment outcomes in AML were also impacted by patient age, morbid obesity, marital status, and payer source in addition to known prognostic disease-specific factors (ELN risk group and t-AML).
This large multi-institutional study has advantages over population-based registries (SEER, NCDB) through incorporation of molecular characteristics, treatment responses and tolerability data not available in public datasets, which can provide insight into biologic intermediates contributing to disparities. Ongoing analyses will examine how variables such as the comorbidity index and measures of socioeconomic status interact with molecular risk factors to determine outcomes in this diverse patient population.
Stock:Research to Practice: Honoraria; Kite, a Gilead Company: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Daiichi: Membership on an entity's Board of Directors or advisory committees; Astellas: Membership on an entity's Board of Directors or advisory committees; Agios: Membership on an entity's Board of Directors or advisory committees; UpToDate: Honoraria. Galvin:Incyte: Consultancy. Altman:prIME Oncology: Speakers Bureau; PeerView: Speakers Bureau; Theradex: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Glycomimetics: Consultancy, Honoraria, Other: Data Safety and Monitoring Committee; Daiichi Sankyo: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Cancer Expert Now: Consultancy; Agios: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy; France Foundation: Speakers Bureau; Abbvie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Biosight: Other: US Lead. Quigley:Alexion: Membership on an entity's Board of Directors or advisory committees; Alnylam: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Dova Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees; TEVA: Research Funding. Khan:Amgen: Consultancy; Celgene: Consultancy; Incyte: Honoraria; Pfizer: Consultancy; Takeda: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal