Background
Laboratory testing is a core component of contemporary medical care. However, repetitive diagnostic phlebotomy has been associated with anemia and higher transfusion burden, both of which are associated with increased mortality. The potential harm of repetitive blood testing is particularly pronounced in the intensive care unit (ICU). Critically ill patients receive a high volume of blood tests due to their need for intensive intervention and monitoring. In addition, ICU patients often suffer from anemia of inflammation which impairs effective erythropoiesis and may exacerbate net red cell loss resulting from repetitive blood testing.
Aim
Modeling data suggests that a 15% decrease in the amount of blood drawn may result in clinically meaningful decrease in ICU anemia.We aimed to reduce the average volume of blood collected per patient-day by 15% by June 30, 2019 by developing and implementing a patient-centered, diagnostic phlebotomy strategy in the Medical-Surgical Intensive Care Unit (MSICU) at an academic tertiary care center in Toronto, Canada.
Methods
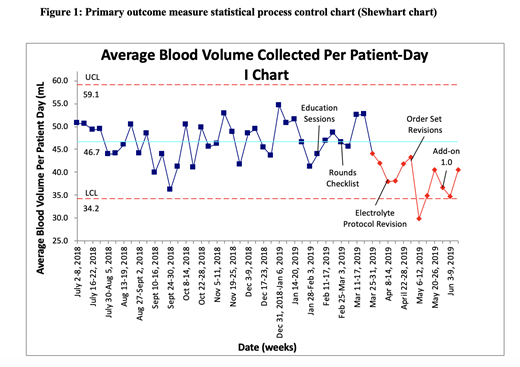
A series of change strategies were implemented in a single-site, 25-bed MSICU between February and July 2019. The strategy included: stake-holder engagement, education sessions, process changes to encourage patient-centered lab ordering, electronic order set modifications to deter open-ended and unnecessary lab ordering, order changes to facilitate add-on testing, and audit and feedback regarding the average volume of blood collected per patient-day in the MSICU. Baseline data from July 2018 to January 2019 was collected retrospectively using administrative data. The main outcome measure was average volume of blood collected per patient-day in the MSICU. Balance measures included average discrete blood draws, ICU length of stay and mortality. The statistical stability of the main outcome measure over time was explored with Shewhart chart (I-chart) analysis. The student's T-Test was also used to compare the mean blood collected per patient-day in the ICU at baseline versus post-intervention.
Results
Baseline data from July 2018 to January 2019 revealed a mean of 46.8 mL of blood was collected per patient-day (including wastage). The volume of blood collected per patient-day was stable during the baseline observation period. Direct observations and process mapping of the blood ordering processes suggested that repetitive and reflexive blood testing was common in the MSICU.
Change strategies were successively introduced between February and June 2019. During the study period average blood volume collected decreased from 46.8ml per patient-day to 36.0 mL per patient day. Special cause variation was observed 6 weeks into the intervention (p < 0.001). The average number of discrete blood draws also decreased from 4.1 to 3.7 per patient day.
Conclusion
Sequential, patient-centered interventions discouraging reflexive and unnecessarily repetitive blood testing in an ICU were associated with a significant decrease in average blood volumes collected per patient-day. Future analyses will explore whether the observed decrease in daily phlebotomy volumes was associated with any changes in patient outcomes such as transfusion burden, ICU length of stay and mortality.
Sholzberg:Novartis: Honoraria; Amgen: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal