Background:
Cancer-associated pulmonary embolism (PE) is a common condition that increases morbidity and mortality among cancer patients. Lymphoma has one of the highest rates of venous thromboembolism in cancer patients. The National Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP) includes the largest all-payer inpatient hospital care data in the United States and therefore may represent a significant sample of clinically relevant pulmonary embolism in lymphoma patients.
Methods:
We utilized the NIS-HCUP database to extract the following data on hospitalizations from 2002 to 2014. We included in our analysis ICD-9 codes for acute PE as a primary or secondary diagnosis of admission and excluded iatrogenic, septic, chronic PE and PE related to obstetrical conditions. We divided our primary population of yielded weighted frequencies i.e. acute PE admissions into two groups: a group with lymphoma as a comorbid condition using Elixhauser comorbidity measures and a group without lymphoma. We identified baseline characteristics of each group including median age on admission, gender and race breakdown as well as common comorbidities' prevalence using Elixhauser comorbidity measures. We ran the analysis for the median length of stay, total charges, mortality scores, readmit scores and inpatient mortality using SAS software, version 9.4 (SAS Institute, Cary, North Carolina). Continuous variables were tested using Wilcoxon two-sample test.
Results:
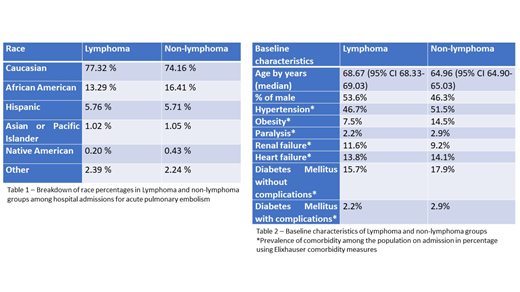
We identified a total of 3,293,040 admissions of acute PE in the database from 2002 to 2014, with 98.5% (3,242,571) of the admissions in patients without lymphoma vs. 1.5% (50,469) in patients with lymphoma as a comorbidity. The breakdown of race was comparable across the two groups with the Caucasian race being predominant in lymphoma and non-lymphoma groups at 77.3% vs. 74.2% respectively [Table 1]. Male gender constituted the majority in the lymphoma group at 53.6% in contrast to the non-lymphoma group where female gender was the majority at 53.6%. [Table 2]. While median age on admission was higher in the lymphoma group compared with the non-lymphoma group (68.7 vs. 65 years respectively) , the prevalence of common comorbidities such as hypertension, paralysis, renal failure, heart failure, diabetes mellitus with and without complications were comparable across the two groups except for obesity prevalence which was higher in the non-lymphoma group. [Table 2]
Median length of stay was marginally but significantly higher in the lymphoma group at 5.4 days (95% CI 5.33-5.53) vs. 4.96 (95% CI 4.95-4.97) days in the non-lymphoma group (p<0.001); as were the readmission scores with a median readmission score of 30 (95% CI 29.65-30.24) vs. 14 (95% CI 13.99-14.08) for lymphoma and non-lymphoma groups, respectively (p<0.001). We observed that total charges of hospitalization were significantly higher in the lymphoma group with a median of 31,899 US dollars (USD) per hospitalization (95% CI 31,174 - 32,622) compared with 27,784 USD (95% CI 27,704 - 27,864) in the non-lymphoma group. Ultimately, all-cause inpatient mortality was higher in the lymphoma group at 10.4% vs. 7.3% in the non-lymphoma group (Odds ratio 1.46, 95% CI 1.43-1.51, P-value <0.0001). Median mortality score was also significantly higher in the lymphoma group at 13.15 (95% CI 12.6-13.6) vs. 5.53 (95% CI 5.50-5.55) in the non-lymphoma group (p<0.001).
Conclusion:
Lymphoma was a comorbid diagnosis in 1.5% of patients admitted to the hospital with acute PE between 2002 and 2014 in the NIS-HCUP database. While the median age in the lymphoma group was higher, the prevalence of clinically significant comorbidities was comparable or higher in the non-lymphoma group. Lymphoma was associated with increased all-cause inpatient mortality in patients admitted with acute PE despite the study's limitation of not excluding other cancer patients from the control non-lymphoma group. Patients in the lymphoma group also had a higher risk of readmission in addition to having higher total charges per hospitalization and increased the length of stay. Efforts should continue to better prevent and treat pulmonary embolism in the lymphoma population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal