The development of venous thromboembolism (VTE) is a known complication occurring in children with leukemia with a reported incidence ranging from 1 to 37% (Ghanem, et al, Pediatric Blood & Cancer, 2017) and can be a source of significant morbidity. Known risk factors for VTE include central venous catheter (CVC) use, thrombophilia, and certain medications, such as asparaginase (Caruso, et al, Blood, 2006.) Despite the known occurrence of VTE in this population, there are no leukemia-specific guidelines for VTE management. Anticoagulant use in children with frequent periods of thrombocytopenia and coagulopathy is not risk free. Various elements of management lack standardization and consensus among practitioners. Given that the majority of pediatric leukemia patients are treated according to standardized protocols, it may be beneficial to standardize anticoagulation care guidelines. Therefore, the primary objective of this study was to assess current practices regarding the management of VTE in the pediatric leukemia population.
We performed a cross sectional, anonymous, electronic survey of members of the American Society of Hematology (ASH) who self-identified as focusing in pediatric hematology or pediatric hematology/oncology, and the pediatric subcommittee of VENUS (VTE Network of the Hemostasis and Thrombosis Research Society) using Qualtrics, a secure online survey tool. Survey items included questions on demographics and clinical practice. Respondents were excluded if they were not board certified/eligible, if they did not participate in patient care, or if they did not answer survey research questions. A $25 gift card incentive was offered anonymously. This study was approved by both the Weill Cornell Medicine and Northwell Health IRBs.
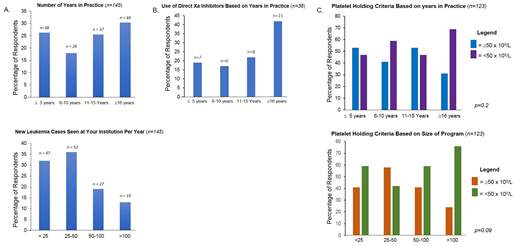
Of 870 surveys distributed, 154 were submitted, giving a 17.7% response rate. Twelve surveys were excluded, leaving 142 surveys for final analysis. There was even distribution of years in practice and size of clinical program among respondents (Figure 1A). Most respondents identified as being in hematology or combined practice.
50% of responding physicians (n=136) reported treating CVC-associated VTE for 3 months. 92% of respondents (n=138) report repeating imaging of the VTE with 58% (n=124) repeating at 6 weeks, and 31% at 3 months. 40% of respondents (n=131) treat cerebral venous sinus thrombosis (CVST) for 3 months, followed by 24% treating for 6 months. 95% of respondents (n=131) repeat imaging for CVST and of these individuals, 40% repeat imaging at 6 weeks followed by 50% at 3 months.
The most frequently utilized anticoagulant class was heparins (n=140); respondents also reported using the direct Xa inhibitors Rivaroxaban (21%) and Apixaban (14%). Within the group utilizing direct Xa inhibitors, those in practice the longest (≥16 years) had the highest percentage of use (Figure 1B.) When asked at what platelet counts they hold therapeutic anticoagulation (n=140), 39% of respondents chose 50 x 109/L, 33% chose 30 x 109/L, and 16% chose 20 x 109/L. One person chose 100, x 109/L, 11% said they did not hold anticoagulation for thrombocytopenia, and 2 respondents gave platelet transfusions rather than hold anticoagulation (one at a cutoff below 30 x 109/L and one below 50 x 109/L). While no significant associations were seen, the highest percentage among individual groups using a platelet cutoff of less than 50 x 109/L were among those in practice longest, and those in the largest centers (Figure 1C).
The results of this survey revealed variation in practice among practitioners regarding VTE management and prevention. Despite the lack of data in this population, a number of physicians are using direct Xa inhibitors in children with leukemia for anticoagulation. Imaging is being done earlier than treatment is being discontinued, potentially implying it is being used to monitor for progression, rather than help guide duration of therapy. Our survey had some limitations, including the low response rate and missing data for questions, which may be due to electronic data collection errors or respondent choice. Recent ASH guidelines endorsed by the Children's Oncology Group propose limited general guidelines and do not consider a cancer patient's unique VTE risk profile. Given the variation seen, multi-center, prospective clinical trials are urgently needed for developing consensus guidelines for the management of VTE in children with leukemia.
Cooley:off-label: Other: drug use. Acharya:Takeda: Membership on an entity's Board of Directors or advisory committees; BioProducts Laboratory: Membership on an entity's Board of Directors or advisory committees; Bayer Pharmaceuticals, LLC: Research Funding; Novonordisk: Membership on an entity's Board of Directors or advisory committees.
Anticoagulations that will be discussed are off-label in children.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal