Introduction: Current stroke prevention guidelines strongly recommend the use of Transcranial Doppler (TCD) screening to detect high risk for ischemic stroke among children with sickle cell anemia (SCA). Despite these guidelines, even recent assessments at sites that participated in the pivotal studies clearly indicate that many children still are not getting screened. DISPLACE (Dissemination and Implementation Looking at the Care Environment) is a multi-center study funded to evaluate and improve optimal implementation of stroke prevention guidelines. Results from Part 1 of DISPLACE (intensive retrospective chart review) determined sub-optimal rates of implementation of TCD screening across sites. To inform effective interventions to improve implementation rates, a multi-level qualitative investigation of barriers and facilitators to obtaining TCD for children with SCA was conducted with patients/caregivers and medical providers. The purpose of this assessment was to identify barriers and facilitators to TCD screening to inform effective interventions in an upcoming phase IV implementation study.
Methods: A qualitative descriptive approach was used to obtain provider and patient/caregiver perspectives through key informant interviews with open-ended questions. Purposive sampling was used to identify patient/caregiver participants and purposive and snowball sampling were used to identify provider participants with the goal of enrolling participants until data saturation was reached. Interviews were digitally audio recorded and transcribed for analysis. Inductive and deductive approaches were used to analyze interview data. Deductive analysis followed the directed content analysis approach with the Multilevel Ecological Model of Health as an initial coding framework. Themes were developed around the barriers and facilitators to TCD screening from an ecological perspective.
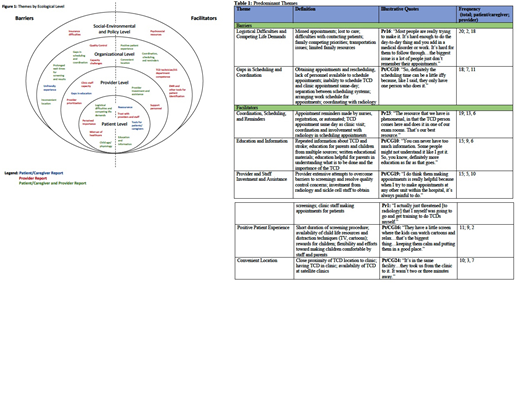
Results: Fifty-two interviews were completed among patients/caregivers (n = 27) and providers (n = 25) to reach data saturation. For patients/caregivers, 26 caregivers of children and adolescents with SCA (mean age = 39; 21 mothers, 4 fathers, and 1 aunt) and one young adult (age 18, female) completed interviews. For providers, 19 physicians, 2 nurse practitioners, 1 physician assistant, and 3 ancillary providers completed interviews (mean age = 50; 14 female; mean years of practice in SCA = 18.8). Patient/caregiver and provider themes were consistent with the multi-ecological framework and reflected barriers and facilitators at the patient, provider, organizational, and social-environmental/policy levels (Figure 1); however, there were some notable differences between patients/caregiver and provider findings. Providers easily identified a much larger range of barriers and facilitators to stroke screening than patients/caregivers whereas the latter group often had to be prompted to consider what might be a barrier or facilitator to TCD screening. Providers, but not patients also reported barriers and facilitators at the social-environmental/policy level. Across patient/caregiver and provider interviews, high frequency or predominant barriers (Table 1) included logistical difficulties and competing life demands (patient level) and gaps in scheduling and coordination (organizational level). High frequency or predominant facilitators included education and information (patient level), provider and staff investment and assistance (provider level), scheduling, coordination, and reminders (organizational level), positive patient experience (organizational level), and convenient location (organizational level).
Conclusions: Patient/caregivers and providers reported a wide range of barriers and facilitators to TCD screening for children with SCA, consistent with the ecological framework. Many of these themes involved interactions across multiple levels (e.g., patient-provider, provider-organizational). This analysis suggests that multi-level interventions involving patients, providers, administrators, and policy makers will be instrumental to improving implementation rates of TCD screening. Specific attention will be given to enhanced coordination and provider-specific interventions in the interventional phase IV study of DISPLACE.
Adams:GBT: Consultancy, Other: consultancy to companies GBT and Blueburd Bio; Bluebird: Consultancy. Kanter:bluebird bio, Inc.: Consultancy; NHLBI: Membership on an entity's Board of Directors or advisory committees; SCDAA: Membership on an entity's Board of Directors or advisory committees; Peerview: Honoraria; Rockpointe: Honoraria; Medscape: Honoraria; Jeffries: Consultancy; Novartis: Consultancy, Honoraria; Imara: Consultancy; Sangamo: Consultancy, Honoraria; Modus: Consultancy, Honoraria; Guidepoint Global: Consultancy; GLG: Consultancy; Cowen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal