Background: GvHD-free, relapse-free survival (GRFS) is a useful composite endpoint that measures survival without relapse or significant morbidity after allogeneic hematopoietic stem cell transplantation (allo-HSCT). We aimed to establish a predictive model of GRFS after allo-HSCT, using a machine learning algorithm within the Kyoto Stem Cell Transplantation Group (KSCTG), a multi-institutional joint research group of 17 transplantation centers in Japan.
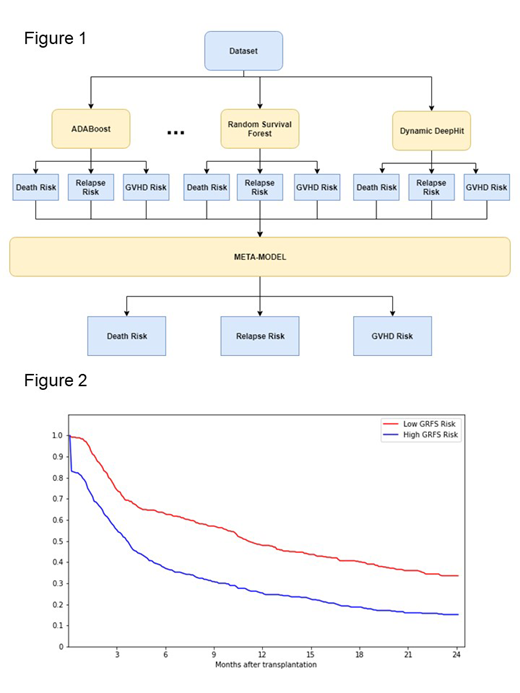
Methods: Consecutive patients with hematologic diseases who had undergone their first allo-HSCT between 1986 and 2016, were included in the study (n = 2,565). The primary endpoint was GRFS, and the secondary endpoints were: overall survival (OS), relapse, non-relapse mortality, and grades II-IV acute GvHD. Data were randomly split into the training set (70% of the dataset) and the validation set (30% of the dataset). The model was trained and tested using a 5-fold cross validation on the training set. A stacking ensemble of multiple machine learning algorithms was applied to develop a model. Predictions were first generated using different machine learning algorithms such as AdaBoost, Random Survival Forest, and Dynamic-DeepHit. A metamodel was subsequently trained using these predictions as inputs, to generate the final prediction (Figure 1). All models were trained using 28 input variables containing information on the patient and transplant characteristics. We used Cox Proportional-Hazards (Cox-PH) model as the benchmark case and evaluated the models' performance using the Harrell's Concordance Index (C-index). The model's final prediction can be directly used as a risk score for each patient. We validated this risk score in the validation set using the competing risk hazard model. Due to the small size of the validation set (N=770), we only classified the final risk scores into 2 groups as follows: high risk (above median) and low risk (below median) for each risk category.
Results: The median age of the patients at transplantation was 48 years (range from 7 to 76). The sources of stem cells were related bone marrow (BM) in 650 patients, related peripheral blood (PB) in 382, unrelated BM in 978, unrelated PB in 24, and cord blood in 522. Myeloablative conditioning was administered in 1,293 patients and reduced-intensity conditioning in 949 patients. Refined disease risk indexes were low in 310 patients, intermediate in 1,197 patients, high in 545 patients, and very high in 368 patients. Median follow-up period of survivors was 4.5 years.
For GRFS, our model achieved a higher C-index across all risk categories (C-index: 0.631) than other top-of-the-art competing risk models (Cox-PH: 0.620, Random Survival Forest: 0.627, Gradient Boosting: 0.609, Component-wise Gradient Boosting: 0.599, Dynamic DeepHit: 0.603). The model also showed the highest C-index for overall survival (C-index: 0.653), relapse (C-index: 0.703), non-relapse mortality (C-index: 0.636), and grades II-IV acute GvHD (C-index: 0.594).
For GRFS, the probability after 1 year and 2 year was 24.9% and 15.2% for the high risk and 48.0% and 33.6% for the low risk, respectively (hazard ratio [HR] compared to the low risk: 1.88; 95% CI: 1.60-2.20) (Figure 2).
The OS at 5 years was 43.4% for the high risk and 70.6% for the low risk (hazard ratio [HR] compared to the low risk: 2.41; 95% CI: 1.96-2.97). The cumulative incidence function (CIF) for non-relapse mortality at 5 years was 32.1% for the high risk and 21.4% for the low risk (HR 2.01; 95% CI: 1.38-2.91). The CIF for relapse at 5 years was 37.1% for the high risk and 16.4% for the low risk (HR 1.67; 95% CI: 1.25-2.23).
Conclusions: A predictive model of GRFS after allo-HSCT was established, which could benefit physicians and patients during the clinical decision-making process. This also forms the basis for research on new prognostic biomarkers by evaluating their predictive power based on our model.
Kanda:MSD: Honoraria; Takeda: Honoraria; Bristol-Meyers Squib: Honoraria; Otsuka: Honoraria; Daiichi Sankyo Company: Honoraria; Novartis: Honoraria; Celgene: Honoraria; Astellas: Honoraria; Chugai: Honoraria; Kyowa Hakko Kirin: Honoraria; JCR Pharmaceuticals: Honoraria; NextGeM Incorporation: Patents & Royalties: 2019-011392. Imada:Bristol-Meyer Squibb K.K.: Honoraria; Celgene K.K.: Honoraria; Otsuka Pharmaceutical Co., Ltd.: Honoraria; Ono Pharmaceutical Co., Ltd.: Honoraria; Kyowa Hakko Kirin Co., Ltd.: Honoraria; Chugai Pharmaceutical Co., Ltd.: Honoraria; Nippon Shinyaku Co.,Ltd.: Honoraria; Takeda Pharmaceutical Co.,LTD.: Honoraria; Novartis Pharma K.K.: Honoraria; Astellas Pharma Inc.: Honoraria. Takaori-Kondo:Takeda: Research Funding; Ono: Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Novartis: Honoraria; Kyowa Kirin: Research Funding; Chugai: Research Funding; Janssen: Honoraria; Pfizer: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal