Abstract
Background Patients with peripheral T cell lymphomas (PTCLs) generally have a poor prognosis with conventional chemotherapy. Most studies demonstrates that, compared to the patients who did not achieve complete remission (CR) after initial therapy, the patients of PTCL who received autologous stem cell lymphoma (ASCT) as consolidation treatment show clearly advantage in survival. However, given the absence of randomized controlled studies, it is unproven that clinical value of consolidative ASCT for PTCL patients achieving CR1. There is a possibility that the survival is similar with or without up-front ASCT group. Thus, we collected the data of PTCL patients who attain CR1 following conventional chemotherapy in our center during the past 10 years. And the objective of this study is to evaluate overall survival(OS), progression-free survival(PFS), and cumulative incidence of relapse (CIR) between observation and first-line ASCT group.
Patients and Methods Weconducted a retrospective study of patients with PTCL who were treated in our center from January 2009 to April 2019. The histopathologic diagnosis of all PTCL patients according to the World Health Organization classification. Exclusion criteria were the following: (1) anaplastic lymphoma kinase (ALK)-positive anaplastic large T-cell lymphoma; (2) cutaneous T cell lymphoma (CTCL); (3) concurrent B cell lymphomas; (4) natural killer/T-cell lymphoma (NK/TCL); (5) patients who underwent allogeneic stem cell transplantation. Furthermore, patients with PTCL age ≤65 years were included. Overall survival(OS )and progression-free survival(PFS) rates were estimated using the Kaplan-Meier method and Survival was compared using the log-rank test. Cumulative incidence of relapse (CIR) was compared by Gray's test competing risk test statistic. The level of statistical significance was set at p < 0.05.
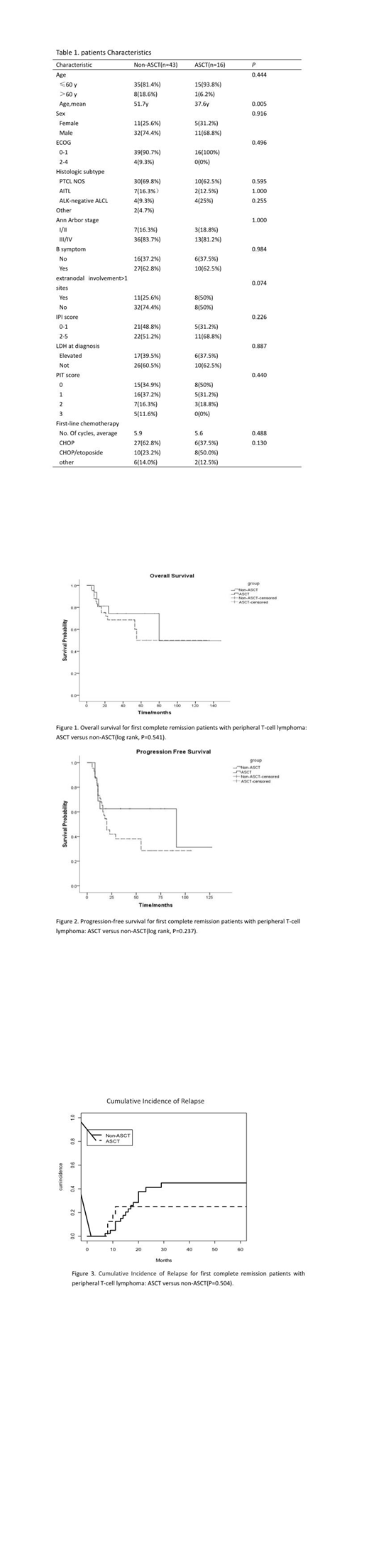
Results A total of 97 patients who met inclusion criteria were enrolled in our center from January 2009 to April 2019. And 59 (59/97, 60.8%)achieved CR1 after receiving induction chemotherapy. Table 1 summarizes the baseline characteristics for the patients in CR1. Of the 59 patients, 43 patients underwent observation and waiting in CR1, 16 patients underwent consolidative ASCT. PTCL NOS accounted for more than 50% at diagnosis in both groups. However, there was significant difference in median age between Non-ASCT group and ASCT group. Patients receiving ASCT were younger and in better physical condition. There were no difference in initial chemotherapy between two groups. Median follow-up time in the entire patient cohort for CR1 (59) was 31months. The median OS and PFS for patients who underwent observation in CR1 was 105 months and 20 months, the median OS and PFS for patients who underwent ASCT as consolidation treatment was 133 months and 91 months. There were no statistical significance in OS (105m vs. 133m, P=0.541) (Figure 1) and PFS (20m vs. 91m, P=0.237) (Figure 2). The estimated 2-year OS was 68.7% and 74.5% in the non-ASCT group and ASCT group, respectively. The estimated 2-year PFS was 41.9% and 62.5%, respectively. When considering incidence of disease relapse, the 2-year cumulative incidence of relapse in the non-ASCT and ASCT group was 41% and 25%, respectively. Again, however, this did not meet statistically significant(P=0.504) (Figure 3). Notably, among patients with advanced-stage disease, elevated LDH, extranodal involvement>1 sites or intermediate-to-high IPI scores, patients who received ASCT as consolidative treatment did not have long time survival compared to the non-ASCT group.
Conclusion In conclusion, for PTCL patients achieving CR1 following induction therapy, consolidative ASCT does not extend overall survival and progression-free survival compared to observation. Similarly, consolidative ASCT also failed to reduce cumulative incidence of relapse. We favor proceeding to observe and wait because of high toxic of hematopoietic stem cell transplantation. However, The finding still needs to be confirmed in a larger, prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal