Introduction: Allogeneic stem-cell transplantation (SCT) is curative therapy in patients with AML or MDS. However, disease recurrence is the major cause of treatment failure. 5-Azacytidine has been used in the standard treatment of MDS and also in the treatment of AML patients not eligible for standard chemotherapy. There is limited data on the safety and efficacy of Azacytidine after SCT. We explored the use of low-dose Azacytidine maintenance therapy for the prevention of relapse of AML/MDS after SCT.
Methods: Patients considered to be at high risk for relapse after SCT were given Azacytidine at 32-50 mg/m2 for 5 days every 28 days for a planned duration of 2 years. Transplantation outcomes were compared with a historical group matched for patient age, disease, status at SCT, cytogenetics, conditioning and donor type. To reduce bias, control patients were required to be alive and in remission for at least the time until the start of Azacytidine prophylaxis in their counterparts. Patients relapsing after SCT and achieving second CR with chemotherapy were also eligible for secondary Azacytidine prophylaxis. The control patients for these patients were also matched for the time from SCT to relapse.
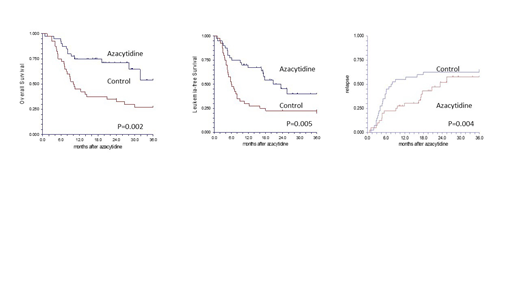
Results: Forty patients, median age 62 years (25-74), 24 male and 16 female, were given azacytidine after SCT from HLA-matched sibling (n=8) or matched-unrelated (n=32) donors. Diagnosis was AML (n=32) or MDS (n=8). The conditioning regimen was myeloablative (n=20) or reduced-intensity (n=20). The status at SCT was untreated MDS/ secondary AML (n=10), CR1 (n=19), CR2 (n=4), refractory AML (n=7). 15 had normal karyotype, 9 complex karyotype and 16 other cytogenetic abnormalities (12 of them high-risk). Fifteen patients were in CR after SCT but at high-risk for relapse due to active disease (n=7) or positive MRD (n=3) at SCT, or poor-risk cytogenetics (n=5). Eight patients were given Azacytidine as secondary prevention after achieving CR with chemotherapy for post-transplant relapse. 17 patients were given Azacytidine pre-emptively for mixed-chimerism (n=9) or positive measurable residual disease (n=8) after SCT. The estimated leukemia-free survival (LFS) in this group of patients is less than 20%. Patients started Azacytidine in a median of 2.2 months (1.2-6.9) after SCT and received a median of 14 courses (1-50). Three patients were also given donor-lymphocyte infusions concomitantly with Azacytidine. 18 patients are still on therapy, 16 died or progressed, 3 stopped after long remission, 2 stopped due to regulatory issues and only 1 had to discontinue due to toxicity. 12 of 23 patients given prophylactic Azacytidine remained in CR, 11 relapsed and 7 of them died. 15 of 17 patients given Azacytidine preemptively achieved a response (10 CR) and 7 remained in CR. 9 died of disease progression and one of non-relapse cause. With a median follow-up of 22.5 months (10.2-45.2), the estimated 3-year overall survival (OS) and LFS rates are 53.9% (95%CI, 29.5-78.4) and 40.0% (95%CI, 21.2-58.6), respectively. In the matched control group, 8 patients are alive, 26 died of relapse and 6 of non-relapse causes. The estimated 3-year OS and LFS rates are 27.1% (95%CI, 13.2-41.0, P=0.002, Figure 1) and 19.7% (95%CI, 7.9-32.1, P=0.005, Figure 2), respectively. The relapse rates were 57.6% (95%CI, 41.6-79.8) and 65.3% (95%CI, 52.0-82.0) in the Azacytidine and control groups, respectively (P=0.04, Figure 3). The median time to relapse was 9.1 months (0.7-25.5) and 4.9 months (1.1-35.9), respectively. The non-relapse mortality (NRM) rates were 2.5% (95%CI, 0.3-17.3) and 15.0 (7.1-31.4), respectively (P=0.01).
Conclusions: Azacytidine is safe and effective therapy when used prophylactically or preemptively in high-risk AML/MDS patients to prevent relapse. Azacytidine maintenance may reduce but more often delay relapse in this high-risk patient group. Azacytidine may also reduce NRM and improve survival in this patient group and should be further explored, possibly in combination with other methods to prevent relapse.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal