Introduction: Viral infections occur more frequently in cord blood transplantation (CBT) than in transplantation of other stem cell sources, and they are often fatal. Thus, it is important to determine the predictors of viral infection to improve CBT outcomes. We hypothesized that incompatibility of human leukocyte antigen (HLA) class I can increase susceptibility to viral infections because donor HLA-restricted naïve cytotoxic T cells cannot recognize recipient infected cells properly in the early term after CBT. Herein, we focused on the impact of HLA class I incompatibility on viral infection within 100 days after CBT.
Patients and Methods: We retrospectively analyzed 121 patients who underwent 126 CBT procedures at Kyoto University Hospital from February 2003 to January 2019. Viral infection was defined as infection of recipient somatic cells by viruses detected via pathology or molecular biology and confined to those specific for an immunocompromised condition. Cytomegalovirus (CMV) antigenemia was distinguished from viral infections, because in such cases, the infected cells are donor-derived cells.
Characteristics were compared between two groups using Fisher's test. The incidences of viral infection, CMV antigenemia, and steroid use for pre-engraftment immune reaction, engraftment syndrome, and acute graft-versus-host disease (aGVHD) together (PIR/ES/aGVHD) were calculated considering death and relapse as competing events, and they were compared using Gray's test. Fine-Gray proportional hazards models were used for univariate and multivariate analyses to evaluate the effects of variables on outcome. Survival was estimated using the Kaplan-Meier method. Non-relapse mortality was estimated using Gray's method.
Results: The median patient age was 47 (range, 19-68) years, and 69 patients were male. The underlying diseases were acute myeloid leukemia (n=53), acute lymphoblastic leukemia (n=17), myelodysplastic syndromes (n=17), anaplastic anemia (n=6), non-Hodgkin lymphoma (n=20), and others (n=9). Regarding the CBT protocol, 44 patients received myeloablative conditioning and 83 patients received a calcineurin inhibitor and mycophenolate mofetil for GVHD prophylaxis. We identified 50 virus infections in 42 transplants within 100 days after transplantation, including 7 human herpesvirus 6 infections, 14 CMV infections, 26 BK virus, JC virus, and adenovirus infections, 2 varicella-zoster virus infections, and 1 unknown virus infection.
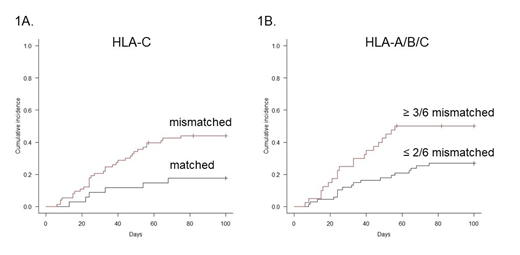
Univariate analysis showed that HLA-A and HLA-C allele mismatches in the GVH direction were associated with a significantly higher incidence of viral infection (mismatch vs. match; HLA-A: 42.7% vs. 25.8%, HR 1.86, P=0.049; HLA-C: 43.9% vs. 17.6%, HR 2.94, P=0.015; Figure 1A). Moreover, 3/6 or more HLA class I allele mismatch in the GVH direction was associated with a significantly higher viral infection incidence (50.0% vs. 26.9%, HR 2.29, P=0.010; Figure 1B), but not with CMV antigenemia (65.8% vs. 70.1%, HR 0.95, P=0.82). These patients with HLA class I mismatches showed no increase in steroid use for PIR/ES/aGVHD (70.4% vs. 64.2%, P=0.53) or prophylactic antiviral drug therapy (62.5% vs. 65.7%, P=0.84). Regarding HLA class II mismatches, HLA-DR mismatch in the GVH direction was not associated with viral infection (34.1% vs. 32.6%, HR 1.13, P=0.72). Univariate analysis showed that lymphoid neoplasm (P<0.01), no use of cytarabine for conditioning (P=0.035), fludarabine and melphalan use for conditioning (P=0.043 and 0.075, respectively), and second or subsequent transplant (P=0.067) were associated with a higher incidence of viral infection. Multivariate analysis showed that HLA class I mismatches and lymphoid neoplasm remained significant factors for viral infection (P=0.035 and <0.01, respectively).
Regarding post-CBT outcomes, 5-year overall survival (OS) and non-relapse mortality (NRM) with landmark analysis at 100 days were inferior in patients with viral infection (OS: 66.5% vs. 73.6%, P=0.35; NRM: 14.6% vs. 4.6%, P=0.11).
Conclusion: HLA class I allele mismatch, including HLA-C mismatch, was significantly associated with viral infection within 100 days of CBT. Our findings suggest the importance of HLA class I genotype compatibility, including HLA-C compatibility, for CBT. Graft matching can reduce the incidence of viral infection and thus improve outcomes.
Kanda:Chugai: Honoraria; Otsuka: Honoraria; JCR Pharmaceuticals: Honoraria; Bristol-Meyers Squib: Honoraria; Kyowa Hakko Kirin: Honoraria; NextGeM Incorporation: Patents & Royalties: 2019-011392; MSD: Honoraria; Daiichi Sankyo Company: Honoraria; Novartis: Honoraria; Celgene: Honoraria; Takeda: Honoraria; Astellas: Honoraria. Takaori-Kondo:Chugai: Research Funding; Janssen: Honoraria; Pfizer: Honoraria; Kyowa Kirin: Research Funding; Novartis: Honoraria; Celgene: Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; Ono: Research Funding; Takeda: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal