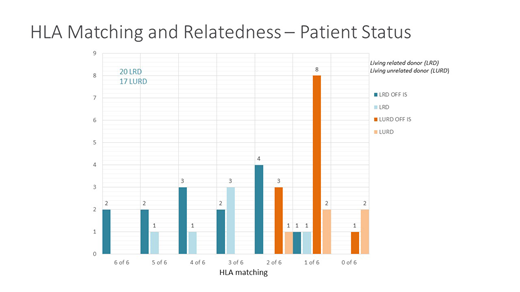
37 patients have been transplanted in a phase 2 protocol to establish chimerism to induce tolerance in up to 0 of 6 matched related and unrelated recipients of living donor renal allografts (KTx). The protocol is based upon tolerogenic CD8+/TCR- facilitating cells (FC) and nonmyeloablative conditioning. Recipients were conditioned with fludarabine (30mg/m2 days -5,-4,-3), cyclophosphamide (50mg/kg day-3 and+3), 200 cGy TBI (day-1) followed by KTx (day0). G-CSF mobilized peripheral blood mononuclear cells were apheresed from the donor >2 weeks before kidney transplantation, processed to remove graft-versus-host disease (GVHD)-producing cells yet retain CD34 +cells and FC, and cryopreserved until transplantation on day+1 after kidney transplantation. Immunosuppression consisted of mycophenolate mofetil and tacrolimus. 36 patients have reached at least 1 year of follow up (range 12-105 months) and are the focus of this analysis. Patients ranged in age from 18-65 yrs. Enrollment was agnostic to degree of HLA match; 2 were 6/6 and 3 5/6 matched related using high resolution allele level typing, with the remainder 4/6 to 0/6 matched related (n=15) or unrelated (n=16) Two of the recipients were renal re-transplants. Tacrolimus/MMF immunosuppression (IS) was weaned and discontinued at 1 year if chimerism (>50% whole blood and T cell), normal renal function and normal kidney transplant biopsy were noted. 34 of 36 subjects exhibited peripheral blood donor chimerism at one month post KTx. Durable chimerism allowing for full IS withdrawal developed in 26 (time off IS from 1- 88 months); the majority (23/26) showed >95% donor whole blood/T cell chimerism. Three have exhibited stable-mixed chimerism ranging between 40% - 60%. Three patients failed to develop chimerism. Transient chimerism occurred in 8 patients. Durably chimeric patients retained chimerism after removal of IS, remain rejection-free without donor-specific antibody (DSA) and show immunocompetence to vaccinations. None have had to resume immunosuppression. Transiently chimeric subjects resumed endogenous hematopoiesis and are maintained on low-dose IS with stable renal function. There have been two cases of GVHD: one grade 2 lower GI acute GVHD that developed during conversion from tacrolimus to sirolimus that responded to steroids; this patient has developed moderate chronic GVHD of the skin. He is off IS. The second presented late following development of severe gastrointestinal symptoms and manifested treatment-resistant lower GI GVHD with associated tissue-invasive CMV colitis that proved fatal at 11 months post-Tx. There have been two additional kidney graft losses, both related to early infections. A second subject death occurred in a heavy (>100 pack yr) smoker who developed advanced stage lung cancer 4.5 years after Tx. A third subject developed pneumococcal sepsis > 4 years after transplant. He had not undergone the recommended pneumococcal vaccination post HSCT. Overall patient survival is 91.8% and death censored graft survival 94.1%. These rates compare favorably to treatment-related mortality rates after standard of care renal transplant. In summary, high levels of durable chimerism and tolerance with a low (5.5%) incidence of GVHD has been achieved in up to 0 of 6 matched related and unrelated recipients of FCR001 + kidney transplant.
Ildstad:Talaris Therapeutics Inc: Employment, Equity Ownership, Other: Founder and CSO.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal