Background
Chimeric antigen receptor therapy (CAR-T) directed against CD19 has demonstrated efficacy in patients with relapsed/refractory (R/R) B-cell malignancies. Delayed hematopoietic recovery with grade 3/4 neutropenia and thrombocytopenia, requiring extended growth factor administration or transfusions, has been observed in patients undergoing CAR-T cell therapy, although the factors influencing recovery are poorly understood. In this study, we performed multivariable analyses to identify factors associated with hematopoietic recovery in patients undergoing CD19 CAR-T cell therapy.
Methods
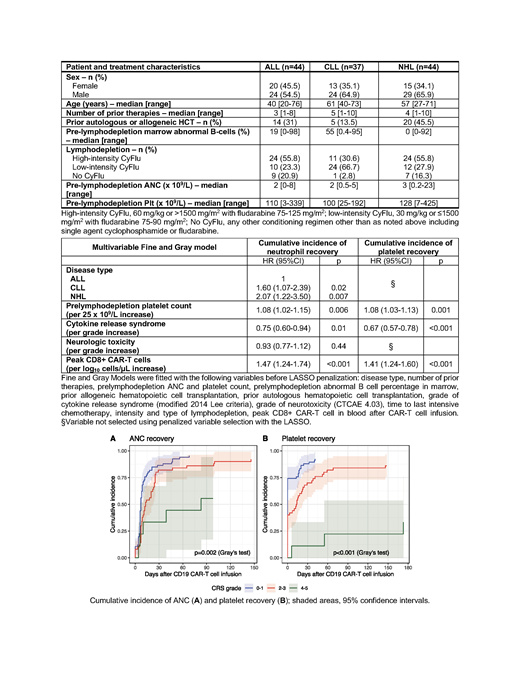
We retrospectively analyzed 125 patients with R/R acute lymphoblastic leukemia (ALL), non-Hodgkin lymphoma (NHL), and chronic lymphocytic leukemia (CLL), treated with CD19-targeted CAR-T cells on a phase 1/2 clinical trial in our institution (NCT01865617). Patients receiving more than one CAR-T infusion were excluded. Criteria for neutropenia, thrombocytopenia, and recovery were defined as per the Center for International Blood and Marrow Transplant Research (CIBMTR) reporting guidelines: neutropenia, absolute neutrophil count (ANC) ≤ 500/mm3; thrombocytopenia, platelet (Plt) count ≤ 20 x 109/L; neutrophil recovery, ANC > 0.5 x 109/L for three consecutive laboratory values obtained on different days irrespective of growth factor administration; platelet recovery, Plt > 20 x 109/L for three consecutive values obtained on different days in the absence of platelet transfusion for seven days. For competing risk analysis, an event was defined as having achieved ANC or Plt recovery, with the following considered as competing events: death, new cytotoxic therapy, relapse with marrow involvement in the absence of ANC or platelet recovery. Patients who never met the CIBMTR criteria for neutropenia of thrombocytopenia were considered as having recovered at time = 0. To identify factors associated with impaired hematopoietic recovery after CD19 CAR-T cell therapy, patient-, disease- and CAR-T cell therapy-related variables were included in a multivariable Fine and Gray model prior to variable selection using LASSO penalization (Table 2 footnote).
Results
We included 125 patients (ALL, n=44; CLL, n=37; NHL, n=44) with a median age of 55 (range, 20-76). Patients were heavily pre-treated with a median of 4 prior therapies (range, 1-10); 31% had undergone prior autologous or allogeneic hematopoietic cell transplantation (HCT). Median ANC and Plt prior to lymphodepletion were 2 x 109/L (range 0-23) and 112 x 109/L, range 3-425), respectively. Patient and treatment characteristics are summarized in Table 1.
ANC and Plt recovery after CD19 CAR-T cell therapy were observed in 91% (ALL, 86%; CLL, 92%; NHL, 95%) and 86% (ALL, 86%; CLL, 86%; NHL, 84%) of patients, respectively. Median time to ANC recovery was 9 days and the probability of ANC recovery at day 28, 60, and 90 was 80% (95%CI, 73-87), 86% (95%CI, 80-92) and 89% (95%CI, 83-94), respectively. The probability of platelet recovery on the day of CAR-T cell infusion was 55% (95%CI, 46-64); rising to 74% (95%CI, 67-82), 83% (95%CI, 76-90), and 84% (95%CI, 77-90) at day 28, 60, and 90, respectively. A competing event was always observed in patients without ANC or Plt recovery.
In multivariable analysis, higher pre-lymphodepletion Plt count (HR=1.08 per 25 x 109/L increase, p=0.006) and higher peak CD8+ CAR-T cells in blood (HR=1.47 per log10 cells/µL increase, p<0.001) were associated with faster ANC recovery. ALL diagnosis and higher cytokine release syndrome (CRS) grade were associated with slower ANC recovery (CLL vs ALL, HR=1.60, p=0.02; NHL vs ALL, HR=2.07, p=0.007). Higher CRS grade was also associated with slower Plt recovery (HR=0.67 per grade increase, p<0.001). Higher pre-lymphodepletion platelet count and higher peak CD8+ CAR-T cell in blood were associated with faster platelet recovery (HR=1.08 per 25 x 109/L increase, p=0.001; HR=1.41 per log10 cells/µL increase, p<0.001). Of note, lymphodepletion intensity did not seem to affect hematopoietic recovery. Table 2 summarizes the results of the multivariable analysis. Figure 1 shows ANC and Plt recovery by CRS grade.
Conclusion
We identified CRS grade as independently associated with impaired hematopoietic recovery after CD19 CAR-T cell therapy. Our findings suggest that the prevention of CRS may improve hematopoietic recovery after CD19 CAR-T cell therapy.
Hirayama:DAVA Oncology: Honoraria. Maloney:Celgene,Kite Pharma: Honoraria, Research Funding; BioLine RX, Gilead,Genentech,Novartis: Honoraria; Juno Therapeutics: Honoraria, Patents & Royalties: patients pending , Research Funding; A2 Biotherapeutics: Honoraria, Other: Stock options . Turtle:Caribou Biosciences: Equity Ownership, Membership on an entity's Board of Directors or advisory committees; Nektar Therapeutics: Other: Ad hoc advisory board member, Research Funding; Allogene: Other: Ad hoc advisory board member; Novartis: Other: Ad hoc advisory board member; Juno Therapeutics: Patents & Royalties: Co-inventor with staff from Juno Therapeutics; pending, Research Funding; Precision Biosciences: Equity Ownership, Membership on an entity's Board of Directors or advisory committees; Eureka Therapeutics: Equity Ownership, Membership on an entity's Board of Directors or advisory committees; T-CURX: Membership on an entity's Board of Directors or advisory committees; Kite/Gilead: Other: Ad hoc advisory board member; Humanigen: Other: Ad hoc advisory board member.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal