Backgound
Venetoclax (V) plus obinutuzumab (O) regimen is active as frontline CLL treatment; a little over half of patients (pts) will achieve undetectable minimal residual disease in the bone marrow (BM-uMRD) with one year of time-limited therapy (Fischer et al. NEJM 2019). Novel strategies may further augment the efficacy of VO. Ibrutinib was previously combined with VO, but relatively high rates of infusion reactions and neutropenia were observed, as were the characteristic toxicities of ibrutinib including diarrhea and bruising (Rogers et al. Blood 2018). Acalabrutinib (A), a more selective BTK inhibitor, is well-tolerated and active as monotherapy or with O, and we previously found that it sensitizes CLL cells to V (Deng et al. Leukemia 2017). We hypothesized that a time-limited triplet combination of A, V, and O (AVO) could achieve a high rate of BM-uMRD with good tolerability. For the first time we now report on the safety and preliminary efficacy data of AVO in previously untreated CLL pts.
Methods
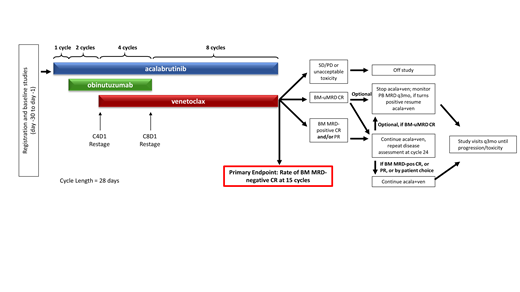
This ongoing open-label, single arm, phase 2 investigator-initiated study (NCT03580928) enrolled pts with previously untreated CLL without restriction by prognostic marker status. Eligibility: requiring treatment by iwCLL criteria, ECOG PS ≤ 2, creatinine clearance ≥50ml/min, absolute neutrophil count ≥500/mm3, and platelets ≥30,000/mm3. A, V, and O are started sequentially (see figure), with one 28-day cycle lead-in with A at 100 mg bid, then 2 cycles of AO (with O at standard dosing), then V ramp-up beginning at C4, followed by 3 more cycles of triplet AVO therapy. After 6 months of O, the AV doublet continues through C15; pts with BM-uMRD-negative CR after C15 may discontinue therapy, while all others continue AV until completing C24, with the option to discontinue therapy if in BM-uMRD CR at that time. Response is assessed by 2018 iwCLL criteria, including bone marrow biopsy with MRD testing in the BM and peripheral blood (PB) by 8-color flow cytometry at a sensitivity of at least 10-4. The primary endpoint is the rate of BM-uMRD CR after 15 cycles. Non-hematologic adverse events (AEs) are assessed by CTCAE v5.0, with hematologic toxicity determined by iwCLL criteria.
Results
The data cut for this interim analysis was July 11, 2019. The study is fully accrued at 37 pts. Median age: 63 years (range: 41-78), 73% male. Baseline prognostic features: unmutated IGHV in 23 (62%) pts, TP53 aberrant disease (defined as either del(17p) and/or TP53 mutation) in 10 (27%) pts, del(11q) in 10 (27%) pts, and complex karyotype in 7 (19%) pts. Thirty-six pts remain on study drugs with a median time on therapy of 8 months (range: 2-11). One pt withdrew consent after 6 cycles due to gastrointestinal symptoms. The overall response rate for the 24 pts who have completed re-staging at C8 is 100%, 18 (75%) PR and 5 (25%) CR. At C8 restaging, 65% of pts were PB-uMRD, 50% of pts were BM-uMRD, and 3 pts (13%) had BM-uMRD CRs. In 8 pts with TP53-aberrant disease who have reached C8, 6 had PR and 2 had CR, with 3 pts BM-uMRD. The most frequent AEs have been fatigue (81% total, 78% gr 1+2, 3% gr ≥3) and headache (76% total, 73% gr 1+2, 3% gr ≥3). Bruising was reported by 16 pts (43%, all gr 1+2). The most frequent gr 3/4 AE has been neutropenia (68% total, 32% gr ≥3). Infusion-related reactions were seen in 8 pts (22%, 19% gr 1+2, 3% gr ≥3). Laboratory tumor lysis syndrome (TLS) occurred in 2 pts (5%), both gr 3 immediately after starting O and prior to any V; both pts continued O. Out of 32 pts, 31 (97%) were medium-to-high risk for TLS on C1D1 but only 3 (9%) were medium-to-high risk at V initiation on C4D1, with 4 medium-to-low risk pts electively admitted for V initiation. One case of gr 3 atrial fibrillation and no cases of hemorrhage or febrile neutropenia were observed.
Conclusion
Our preliminary data suggest that even at an early response evaluation after 8 cycles of therapy (including only 4 months of V), AVO as frontline CLL therapy leads to a high proportion of pts achieving BM-uMRD and CR, including pts with TP53-aberrant disease. The AE profile is favorable, with a low rate of infusion reactions and no significant cardiac or bleeding toxicities. Updated data will be presented at the meeting for this ongoing study. Based on our initial results we have opened an expansion cohort to further characterize the efficacy and safety of AVO. AVO will also be studied head-to-head against chemoimmunotherapy and the AV doublet in the phase 3 trial CL-311 (NCT03836261), which is currently enrolling.
Montegaard:Pharmacyclics: Consultancy; Janssen: Consultancy. Jacobson:Kite, a Gilead Company: Consultancy, Honoraria, Other: Travel Expenses, Research Funding; Novartis: Consultancy, Honoraria, Other: Travel Expenses; Pfizer: Consultancy, Research Funding; Humanigen: Consultancy, Other: Travel Expenses; Bayer: Consultancy, Other: Travel Expenses; Precision Biosciences: Consultancy, Other: Travel Expenses; Celgene: Consultancy, Other: Travel Expenses. Jacobsen:Astra-Zeneca: Consultancy; Novartis: Research Funding; F. Hoffmann-LaRoche: Research Funding; Takeda: Honoraria; Pharmacyclics: Research Funding; Merck: Consultancy, Research Funding; Acerta: Consultancy. LaCasce:Seattle Genetics: Consultancy, Research Funding; BMS: Consultancy; Research to Practice: Speakers Bureau; Humanigen: Consultancy. Arnason:Regeneron Pharmaceuticals, Inc.: Consultancy; Celgene/Juno: Consultancy. Armand:Merck: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Bristol-Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Adaptive: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Affimed: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche: Research Funding; Otsuka: Research Funding; Sigma Tau: Research Funding; Infinity: Consultancy; Genentech: Research Funding; Pfizer: Consultancy; ADC Therapeutics: Consultancy; Tensha: Research Funding. Brown:BeiGene: Consultancy; AbbVie: Consultancy; Catapult Therapeutics: Consultancy; Dynamo Therapeutics: Consultancy; Genentech/Roche: Consultancy; Kite, a Gilead Company: Consultancy, Research Funding; Loxo: Consultancy, Research Funding; Novartis: Consultancy; Juno/Celgene: Consultancy; Acerta Pharma: Consultancy; AstraZeneca: Consultancy; Gilead: Consultancy, Research Funding; Pfizer: Consultancy; Pharmacyclics: Consultancy; Sunesis: Consultancy; TG Therapeutics: Consultancy; Verastem: Consultancy, Research Funding; Sun Pharmaceuticals: Research Funding; Janssen: Honoraria; Teva: Honoraria; Morphosys: Other: Data safety monitoring board; Invectys: Other: Data safety monitoring board; Octapharma: Consultancy. Davids:AbbVie, Acerta Pharma, Adaptive, Biotechnologies, Astra-Zeneca, Genentech, Gilead Sciences, Janssen, Pharmacyclics, TG therapeutics: Membership on an entity's Board of Directors or advisory committees; AbbVie, Astra-Zeneca, Genentech, Janssen, MEI, Pharmacyclics, Syros Pharmaceuticals, Verastem: Consultancy; Acerta Pharma, Ascentage Pharma, Genentech, MEI pharma, Pharmacyclics, Surface Oncology, TG Therapeutics, Verastem: Research Funding; Research to Practice: Honoraria.
Acalabrutinib, venetoclax, obinutuzumab - combination therapy for previously untreated CLL
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal