Background: In the S0777 phase 3 trial (Durie et al., Lancet. 2017), the lenalidomide, bortezomib, and dexamethasone (RVD) triplet showed survival advantage over lenalidomide/dexamethasone (RD) as initial therapy for myeloma. However, older transplant-ineligible patients often receive doublet regimens (RD or bortezomib/dexamethasone [VD]), or VD plus cyclophosphamide (VCD). In this setting, RVD has not been directly compared with doublets, or RD compared with VD, leaving an important gap in evidence. Our objective was to compare these regimens based on real-life data from older patients receiving first-line therapy for myeloma in the United States (US), using a causal inference approach.
Methods: We identified Medicare beneficiaries with myeloma receiving first-line RD, VD, RVD, or VCD in 2007-2015, using Medicare claims linked to data from cancer registry (SEER-Medicare) covering ~35% of the US population, with successful linkage of >95% individuals aged 65 or over. Patients had to have complete Medicare claims, including outpatient prescriptions (Part D), and we excluded cases with amyloidosis or end-stage renal disease. We used propensity score analysis to generate pseudo-randomized cohorts balancing multiple baseline factors, including socio-economic and performance status, time from diagnosis, presence of baseline hypercalcemia, renal disease, anemia, neuropathy, venous thromboembolism (VTE), and other comorbidities. In each comparative analysis, we fitted a separate propensity score, aiming at confounder balance measured by standardized difference of means <0.10. After generating adequately balanced cohorts to minimize indication bias, we analyzed two survival endpoints (measured from start of first-line therapy): event-free survival (EFS, defined as start of a 2nd-line agent, hospice enrollment, or death, censored in case of an autologous transplant) and overall survival (OS), reporting hazard ratios (HR) with 95% confidence intervals (CI). We also compared select identifiable toxicities occurring within 6 months of starting therapy: hospitalization, anemia, neuropathy, and VTE, reporting relative risk (RR), as well as cumulative incidence function (CIF) for secondary solid tumors, reporting subhazard ratio (SHR).
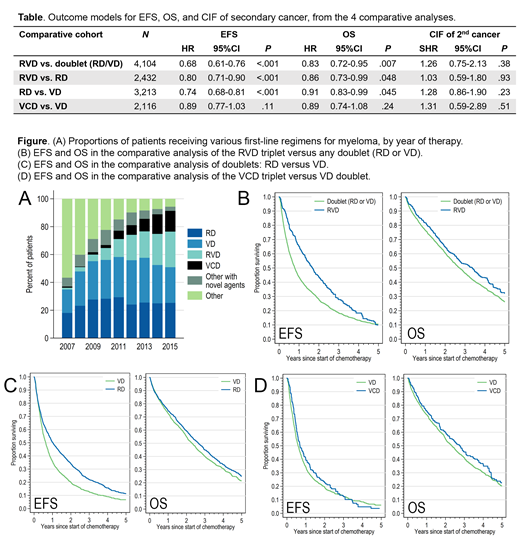
Results: We identified 6,076 eligible myeloma patients receiving first-line therapy between 2007 and 2015. Median age was 76 years [y], and there were 50% women. Between 2007 and 2015, the proportion of Medicare beneficiaries receiving RD increased from 18% to 25% (total N = 1,541; Fig. A), VD from 17% to 26% (N = 1,672), and RVD from 1% to 26% (N = 891). Median EFS in the study population was 0.88 y (95%CI, 0.83-0.93), and median OS was 2.7 y (95%CI, 2.6-2.8 y). Lenalidomide was dosed at 25mg in 58%. Bortezomib was dosed weekly in 57%.
Detailed results of comparative models are shown in the Table. In the analysis of RVD versus (vs.) doublets, RVD showed better EFS (median 1.7 vs 0.8y; Fig. B) and OS (median 3.4 vs 2.7y). RVD resulted in higher rates of hospitalization (RR, 1.17; 95%CI 1.03-1.32), anemia (RR, 1.16; 95%CI 1.09-1.23), and neuropathy (RR, 1.49; 95%CI, 1.14-1.96), but no increased risk of VTE (RR, 1.06; 95%CI, 0.79-1.44). A higher proportion of patients treated with RVD underwent consolidative transplant (26% vs 6%). There was no significant difference in the risk of secondary cancers. Consistent findings were observed in the more specific comparison of RVD vs. RD (Table).
In the analysis of RD vs. VD, RD demonstrated better EFS (median 1.0 vs 0.6y; Fig. C) and marginally better OS (median 2.7 vs 2.3y). RD resulted in more frequent VTE (RR, 1.44; 95%CI, 1.13-1.83), but less neuropathy (RR, 0.39; 95%CI, 0.29-0.53), without significant difference in hospitalization (RR, 0.96; 95%CI, 0.87-1.06) or anemia (RR, 0.95; 95%CI, 0.89-1.00).
In the comparison of VCD vs. VD, there were no significant differences in EFS (Fig. D), OS, or observed toxicities.
Conclusions: In this large, population-based study, first-line RVD shows EFS and OS advantage for older patients with myeloma who can tolerate higher potential short-term toxicity. RVD (or "RVD-lite" to minimize toxicity) should be the preferred regimen, but it is applied in only a minority of Medicare beneficiaries. For patients not eligible for the RVD triplet, an unexpected advantage of RD over VD was observed, suggesting that RD may be the preferred doublet. VCD appears to offer no benefit over the VD doublet.
Olszewski:Spectrum Pharmaceuticals: Research Funding; Genentech: Research Funding; TG Therapeutics: Research Funding; Adaptive Biotechnologies: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal