Background Deferasirox (DFX) is widely employed as iron chelation therapy (ICT) in the current clinical practice in patients with myelodysplastic syndromes (MDS) and chronic transfusion need. The efficacy of DFX in reducing median ferritin levels in different cohorts of these patients has been reported in many trials, but the lack of worldwide accepted criteria of individual response to ICT makes it difficult to appreciate its clinical relevance for any single patient.
Aim To highlight the clinical impact of ICT with DFX in a large real-life cohort of MDS patients, based on different individual ferritin variation during treatment.
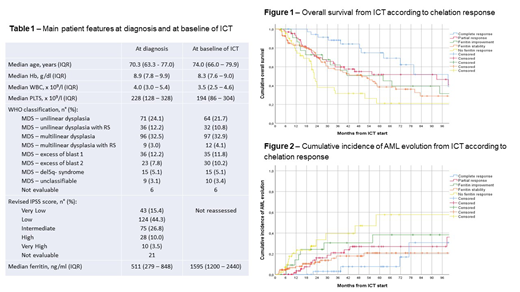
Methods A retrospective cohort of 301 consecutive MDS patients [M/F 187/114 (62.1%/37.9%)] of any age followed in 20 hematological Centers in Italy was analyzed: the main features at diagnosis are reported in the Table 1. Individual response to ICT was categorized as complete response (CR) (ferritin levels < 500 ng/ml), partial response (PR) (ferritin levels < 1,000 ng/ml), ferritin improvement (FI) (ferritin reduction > 50% of baseline value but with levels > 1,000 ng/ml), ferritin stability (FS) (ferritin levels without changes from baseline during ICT) or no ferritin response (NR) (ferritin levels increasing during ICT).
Results ICT was started after a median period from diagnosis and from transfusion start of 21.0 months [interquartile range (IQR) 8.9 - 44.3] and 11.3 months (IQR 7.1 - 21.7), respectively, with a median burden of red cell transfusions at baseline of 22 units (IQR 14 - 35). The main features of patients at baseline of ICT are reported in the Table 1. Starting DFX dose was < 10 mg/Kg in 38 patients (12.7%), 10 - 14 mg/Kg in 110 patients (36.6%), 15 - 19 mg/Kg in 57 patients (18.9%) and ≥ 20 mg/Kg in 96 patients (31.9%). As to individual response, 4 patients (1.3%) were too early for evaluation (< 6 months of DFX treatment): in addition, 16 patients (5.4%) discontinued ICT behind 6 months from start, due to early toxicity (10 patients, 7 for gastro-intestinal toxicity and 3 for skin toxicity) or other reasons (unrelated death, AML evolution, transplant procedure). Among the remaining 281 patients, 37 (12.3%) achieved a CR, 65 (21.6%) a PR, 23 (7.6%) a FI, 112 (37.2%) a FS and 44 (14.6%) a NR. Five-year overall survival (OS) of the whole cohort from ICT start was 43.9% (95%CI 37.1 - 50.7). Five-year OS according to ICT response was 74.8% (95%CI 57.9 - 91.7) in patients with CR, 51.7% (95%CI 37.6 - 65.8) in patients with PR, 50.6% (95%CI 28.2 - 73.0) in patients with FI, 38.6% (95%CI 27.0 - 50.2) in patients with FS and 21.1% (95%CI 5.2 - 37.0) in patients with NR (p=0.002) (Figure 1). Five-year cumulative incidence of AML evolution (CIE) of the whole cohort from ICT start was 27.1% (95%CI 20.3 - 33.9). Five-year CIE according to ICT response was 7.6% (95%CI 0 - 18.0) in patients with CR, 27.0% (95%CI 13.0 - 40.5) in patients with PR, 38.3% (95%CI 15.5 - 61.7) in patients with FI, 20.8% (95%CI 10.4 - 31.2) in patients with FS and 57.7% (95%CI 31.9 - 83.5) in patients with NR (p=0.003) (Figure 2). Notably, no statistical difference was observed for both OS and CIE among patients achieving PR, FI or FS.
Conclusions Present data highlight the clinical relevance of individual response in MDS patients receiving ICT with DFX. In particular, achievement of CR seemed related to a better OS and a lower CIE, while patients with NR had a significant worst OS and CIE: furthermore, the achievement of stable ferritin levels was associated with similar OS and CIE than PR and FI and thus should be considered as a response.
Latagliata:Celgene: Honoraria; Janssen: Honoraria; Novartis: Honoraria; Pfizer: Honoraria. Oliva:Novartis: Consultancy, Speakers Bureau; Celgene Corporation: Consultancy, Honoraria, Speakers Bureau; Apellis: Consultancy. Pilo:Novartis: Other: Advisory board. Molteni:Celgene: Membership on an entity's Board of Directors or advisory committees. Balleari:Celgene: Membership on an entity's Board of Directors or advisory committees. Breccia:Novartis: Honoraria; BMS: Honoraria; Pfizer: Honoraria; Incyte: Honoraria; Celgene: Honoraria. Foà:Incyte: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celltrion: Membership on an entity's Board of Directors or advisory committees; Abbvie: Consultancy, Speakers Bureau; Roche: Consultancy, Speakers Bureau; Incyte: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Roche: Consultancy, Speakers Bureau; Celltrion: Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Shire: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Consultancy, Speakers Bureau; Shire: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Finelli:Novartis: Consultancy, Speakers Bureau; Janssen: Consultancy, Speakers Bureau; Celgene Corporation: Consultancy, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal