Background: Providing achievement and sustainability of deep molecular responses (DMR), patients (pts) taking tyrosine kinase inhibitors (TKI) against CML may discontinue therapy. The STOP 2G-TKI observational study showed that dasatinib and nilotinib could be safely stopped and prior suboptimal response or resistance to imatinib was an adverse prognostic factor for treatment-free remission (TFR). We present updated results with a specific focus on the risk of relapse using post-baseline information during follow-up.
Methods: Adult CML pts treated with dasatinib or nilotinib without a history of allogeneic stem cell transplantation (ASCT) or progression to advanced phase stopped TKI provided that: (1) BCR-ABL transcripts were of the major type, (2) total TKI treatment duration was ≥36 months, (3) uMR4.5 had been achieved and maintained for ≥24 months (undetectable BCR-ABL with ≥32000 copies of ABL). Relapse was defined by loss of major molecular response (MMR: BCR-ABL IS >0.1%) on a single occasion and triggered TKI reintroduction. The primary objective was TFR at 12 months. After TKI discontinuation, BCR-ABL transcripts were monitored monthly during the first 6-12 months, every 3 months during the 2nd year and then every 3-6 months. Data as of July 1, 2019 are reported in 104 pts (median follow-up 55 months (range: 6-70)).
Results: Median age at inclusion was 56 years (range: 21-82) and 65.4% of pts were female. Sokal risk score was low in 49%, intermediate in 31%, high in 16% and unknown in 4%. 2G-TKIs were given after imatinib intolerance in 47% of pts, suboptimal response or resistance to imatinib in 22%, lack of DMR on imatinib in 3% and as 1st line treatment in 28%. Median duration of TKI, 2G-TKI and uMR4.5 was 74 months (range: 36-163), 49 months (range: 19-112) and 31 months (range: 24-72), respectively.
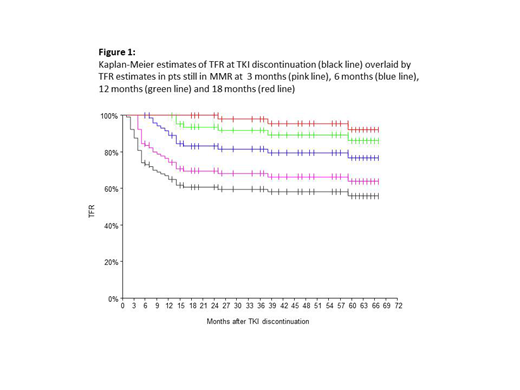
Overall, 43 pts (41%) lost MMR within a median time of 5 months (range: 1-59). Overall 60-month TFR was 56% (95% CI, 45.8-66.3) but TFR probabilities increased up to 64% (95% CI: 53.3-74.8), 76.7% (95% CI, 65.9-87.5), 86.2% (95% CI; 76.3-96.2), and 92.1% (95% CI: 83.4-100) for pts still in MMR at 3, 6, 12 and 18 months, respectively (Figure 1).
Prior suboptimal response or resistance to TKI was confirmed as the strongest adverse baseline prognostic factor with a 60-month TFR rate of 29.8% (95% CI; 10.8-48.7) (median TFR 12 months) versus 63.6% (95% CI; 52.1-75.2) (median not reached) in pts without such history (logrank p=0.0012). This was explained by significantly higher risk of early relapses (within 6 months but not later) in pts with prior suboptimal response or resistance to TKI (cumulative incidence of relapses by 6 months 47.8% (95% CI; 31.2-73.2) versus 20.9 (95% CI; 13.7-32) in other pts (p=0.00879)).
Landmark analyses at specific time points were performed to study the prognostic value of molecular responses categories after TKI discontinuation. All pts in MMR but not deeper at 3 months relapsed by month 9 (median time to relapse 4 months) while pts in ≥MR4 (BCR-ABL IS ≤0.01%) had 12- and 60-months probabilities of 86.8% (95% CI; 79.1-94.4) and 74.9% (95% CI: 64-85.7), respectively (logrank p<10-4). All pts but 1 in MMR but not deeper at 6 months relapsed (median time to relapse 12 months) while pts in ≥MR4 had 12- and 60-months probabilities of 95% (95% CI; 89.6-100) and 87.5% (95% CI: 78.7-96.2), respectively (logrank p<10-4).
Forty three pts restarted treatment including 1 who lost MR4.5 but not MMR and 42 who lost MMR. When treatment was reintroduced, 42 pts were in CHR and all regained MMR after a median time of 3 months (range: 1-11). The remaining pt lost MMR but not CHR 5 month after 1st line nilotinib cessation and was found in sudden myeloid blast crisis at the month 6 TKI reintroduction visit. No BCR-ABL mutation was found but an inversion of chromosome 3 at karyotyping analysis. The pt underwent ASCT after chemotherapy + ponatinib and is alive in remission 29 months later.
Conclusion: 2G-TKI may be successfully stopped in CML pts with long-lasting MR4.5. Those without a history of suboptimal response or resistance have greatest chances of success. Sudden blast crisis is rare but unpredictable. Post-TKI discontinuation estimates of TFR change overtime. Together with that of molecular response type at specific time points, they represent important dynamic prognostic measures of outcome. They may also help individualizing molecular monitoring programs after TKI cessation.
Rea:Incyte Biosciences: Honoraria; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; BMS: Honoraria; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees. Nicolini:Sun Pharma Ltd: Consultancy; Incyte Biosciences: Honoraria, Research Funding, Speakers Bureau; Novartis: Research Funding, Speakers Bureau. Rousselot:Pfizer: Research Funding; Incyte: Research Funding. Etienne:Pfizer: Honoraria, Speakers Bureau; Incyte Biosciences: Honoraria, Speakers Bureau; BMS: Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau. Guerci:INCYTE: Consultancy, Honoraria. Legros:Pfizer: Honoraria, Research Funding; BMS: Honoraria; Novartis: Honoraria; Incyte Biosciences: Honoraria, Research Funding. Coiteux:Pfizer: Honoraria; BMS: Honoraria; Novartis: Consultancy, Honoraria; Incyte: Consultancy, Honoraria. Mahon:Pfizer: Honoraria, Speakers Bureau; BMS: Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau; Incyte Biosciences: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal