Background: Post-transplant lymphoproliferative disorders (PTLD) represent a heterogeneous group of immune-deficiency related lymphoid malignancies occurring after solid organ transplant (SOT) or bone marrow transplant. Monomorphic PTLD (mPTLD) is typically characterized by diffuse large B-cell lymphoma (DLBCL), though other mature B and T-cell lymphomas make up a small contribution. In one of the largest prospective clinical trials in PTLD, Trappe et al described a risk stratified sequential treatment approach using rituximab (R) monotherapy induction followed by either (R) consolidation or chemoimmunotherapy (chemoR) based on interim response. The role of cytogenetic and immunohistochemistry (IHC) risk stratification have not been fully described in mPTLD. In this study, we aim to identify clinical factors which may lead to differences in clinical outcomes in mPTLD.
Methods: Pts diagnosed with mPTLD following SOT at the University of North Carolina at Chapel Hill were identified by an IRB approved EMERSE query of the medical record. Histologic classification was determined by pathologist review at the time of diagnosis. DLBCL subtype was determined as either germinal center B-Cell (GCB) type, non-GCB type, or unclassifiable using Hans IHC criteria. Double-Hit lymphoma (DHL) was defined as the presence of a MYC rearrangement in combination with either a BCL2 or BCL6 rearrangement by in-situ hybridization. Double expressor lymphoma (DEL) was defined as the presence of MYC and BCL2 co-expression by IHC. Additional copies of MYC or BCL2 were determined by in-situ hybridization. Clinical responses were determined per Lugano criteria. Cox regression was used to evaluate the association of covariates of interest with overall survival (OS).
Results: A total of 29 pts were diagnosed with mPTLD between 2010 and 2019. The median age at diagnosis was 55 years (range, 19-84 years). Transplanted organs included 16 kidney (56%), 5 lung (17%), 4 liver (14%), 3 heart (10%), and 1 kidney/heart (3%). The median time from transplant to diagnosis was 7.1 years (range, 0.2 to 24.5 years). Sub-classification of mPTLD revealed 11 non-GCB type (38%), 10 GCB type (35%), 7 unclassifiable DLBCL (24%), and 1 PTCL (3%). EBV encoded RNA (EBER) in-situ hybridization was positive in 10 pts (35%) and concurrent EBV reactivation was detected in 7 of the 10 pts.
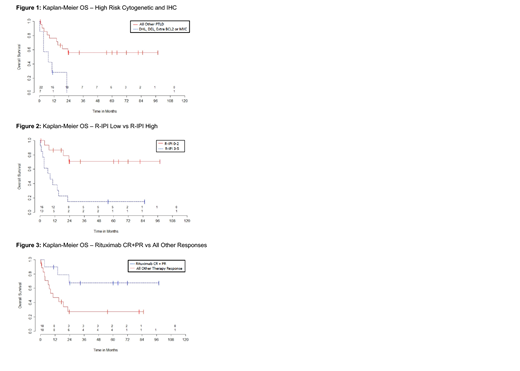
Both categorized EBV encoded RNA (EBER) in-situ hybridization, and GCB vs non-GCB type mPTLD did not appear to be significantly associated with OS. mPTLD that was DHL (1 pt), DEL (3 pts), or had extra copies of MYC/BCL2 (3 pts) had significantly shorter OS (p=0.006, Figure 1). The 1 year OS for those with high risk cytogenetics and IHC was 29% [95% CI: 4% to 61%] versus those without at 76% [52% to 89%]. Consistent with prior studies, pts with revised International Prognostic Index (R-IPI) high (3-5) had a significantly shorter OS (p=0.001, Figure 2). The 1 year OS for those with dichotomized R-IPI high was 38% [95% CI: 14% to 63%] versus those with R-IPI low at 87% [95% CI: 56% to 96%].
All pts had a reduction in immunosuppression at diagnosis. Fourteen pts (48%) were treated with front-line (R) monotherapy. Seven of these pts achieved a CR (50%), 3 pts achieved a PR, 3 pts developed progressive disease and 1 pt died during therapy. Eleven pts (38%) were treated with front-line chemoR. Seven of these pts achieved a CR, 3 pts achieved a PR, and 1 pt died during therapy. Pts who achieved a CR or PR with (R) monotherapy induction had a better OS compared to pts who either had no response to (R) or were treated with chemoR (p=0.01, Figure 3). The 1 year OS for (R) CR/PR was 90% [47% to 99%] versus all other pts including those treated with combination chemoR at 47% [23% to 68%]. Of note, pts who achieved a CR with either (R) induction or chemoR in the front-line setting had borderline significantly improved OS (p=0.06).
Conclusion: Response to therapy within mPTLD is quite variable. In this study, we reveal a population of mPTLD with particularly poor outcomes (DHL, DEL, and extra copies of MYC/BCL2). To our knowledge, this is the first study to show the dramatic impact of poor risk cytogenetic and IHC findings on clinical outcomes in mPTLD. As seen in other cohorts, high R-IPI score was associated with poor outcomes. Objective response to (R) induction in the front-line setting was associated with improved survival.
Grover:Seattle Genetics: Consultancy. Dittus:Seattle Genetics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal