Background: The number of solid organ transplantation (SOT) is increasing. While the remarkable improvement in SOT procedures provides recipients with a good chance of long-term survival, the prolonged immunosuppression has led toa variety of malignancies in solid organ transplant (SOT) recipients; post-transplant lymphoproliferative disorder (PTLD) is a life-threating complication among them. However, there remain some controversies regarding its clinical features.
Method: We retrospectively surveyed the patients who had visited both departments: hematology and urology, or renal surgery in kidney center at Tokyo Women's Medical University Hospital from 2003 to 2017. We identified 61 patients diagnosed with hematological disorder in kidney-transplant recipients. Among them, PTLD were analyzed. Continuous variables were compared using Student's t-tests. Overall survival rate (OS) was calculated using the Kaplan-Meier method. P values < 0.05 were considered significant. Statistical analyses were performed using JMP Pro 14 (SAS Institute Inc., Cary, NC, USA) and GraphPadPrism version 7.0 (GraphPad Software, San Diego, USA). This study was conducted in accordance with the Declaration of Helsinki and approved by the institutional review boards.
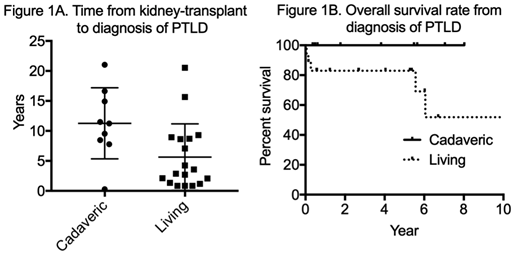
Results: During the survey period, 3,133 patients had visited both departments: hematology and urology, or surgery in Kidney Center. Among them, 61 kidney-transplant recipients were diagnosed with hematological disorder; they comprised 27 PTLD, 10 plasmacytic disorder, 6 idiopathic thrombocytopenic purpura, 5 myelodysplastic syndromes, 4 acute leukemia, 3 polycythemia, 6 other diseases. Among the patients with PTLD (n = 27), 18 patients (66.7%) were male.Median patient ages at the diagnosis of PTLD and kidney transplant were 54 (25-79) and 43 (16-75) years, respectively. Eighteen and nine patients had received kidney-transplant from a living donor (15 related and three unrelated donors) and a cadaveric donor, respectively. The median time from kidney transplant to diagnosis of PTLD was 7.8 years; there was a significant difference in the time between the kidney-transplant recipients from a cadaveric donor and those from a living donor (Figure 1A, 11.3 and 5.6 years, P = 0.02). With regard to the histological subtypes of PTLD, they comprised 17 diffuse large B-cell lymphoma (63.0%), 2 Burkitt lymphoma (7.4%), 4 unclassified B-cell lymphoma (14.8%), 2 T-cell lymphoma (7.4%), and 2 unknown cases (7.4%). 24 of 27 patients had extranodal involvement: 9 central nervous system (33.3%), 7 gastrointestinal tract (25.9%) and other sites. First-line treatment procedure which all patients received was the modification of immunosupressants; complete response (CR) rate was 37.0%. After the failure of first-line therapy, 15 of 27 patients received chemotherapy: 4 rituximab monotherapy (30.8%), 6 CHOP-like regimens (46.2%), and other regimens (33.3%). Among them, five patients experienced relapse. They received salvage chemotherapy, and 2 and one patients achieved CR and partial response, respectively. Rest of them died of lymphoma and infection. The estimated five-year OS from the diagnosis of PTLD and the initiation of chemotherapy was 88.7% and 86.7%, respectively. During the survey period, 5 patients died; their causes of death were 3 lymphomas, 1 infection, and 1 heart failure. There were no deaths in kidney-transplant recipients from a cadaveric donor (Figure 1B).
Discussion: While our cohort had more extranodal PTLD recipients than those reported previously, the modification of immunosupressants improved them in more than one-third of cases, which showed the usefulness of it as first-line treatment procedure for PTLD. Nearly half of cases were identified in recipients from a cadaveric donor; the results suggest that the incidence o PTLD among them is higher than those from a living donor because the number of kidney-transplant from a living donor was 10 times higher than those from a cadaveric donor. This study has several limitations due to its retrospective nature and small sample size. In addition, the estimated five-year OS might be better than actual because some patients became lost to follow-up. Further large-scale studies are warranted to validate the findings of this study.
Hagiwara:Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees. Tanaka:Bristol-Myers Squibb: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal