Chromosomal abnormalities are established prognostic markers in adult ALL. Analysis of the UKALLXII/ECOG2993 trial (Blood, 2007;109:3189) revealed that patients (15-65 years) with BCR-ABL1, KMT2A-AFF1, low hypodiploidy (HoL) or a complex karyotype (CK) had a significantly inferior outcome in multivariable analysis. In UKALL14 (ISRCTN 66541317), all patients (25-65 years) with these genetic abnormalities were stratified to the high-risk arm to receive allogeneic stem cell transplant (alloSCT), where possible, or an unrelated transplant. Patients with BCR-ABL1 received imatinib.
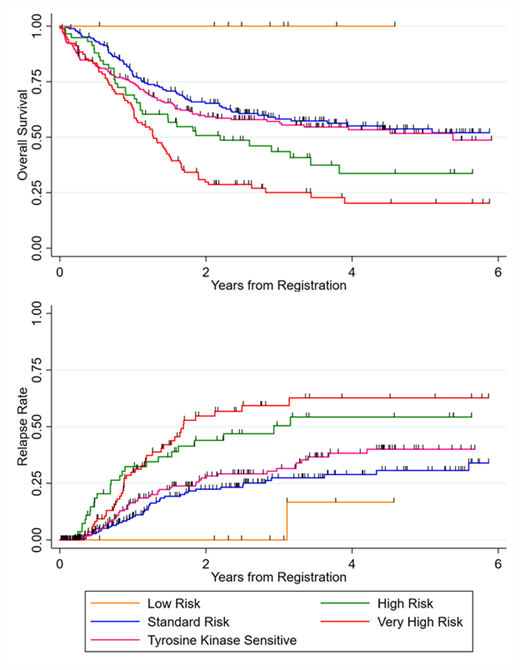
The objectives of this study were to determine the frequency and outcome of patients with high-risk chromosomal abnormalities and identify new high-risk genetic abnormalities by screening for novel gene rearrangements and copy number alterations. All genetic screening was performed using diagnostic marrow samples and by cytogenetics, FISH and MLPA. Survival endpoints were defined according to the trial protocol and analysed using standard statistical methods. After a median follow-up time of 3.4 years the 3 year survival rates for the whole B-cell precursor ALL cohort were: overall survival (OS) 52% (95% 48-56), event-free survival (EFS), 45% (41-49), relapse rate (RR) 34% (30-39).
Among 653 patients, 319 (49%) harboured high-risk primary chromosomal abnormalities: BCR-ABL1 (197/635, 31%), KMT2A-AFF1 (49/616, 8%), HoL (49/525, 9%), and CK (21/512, 5%). The OS of patients with CK and HoL was 24% (95% CI 9-43) & 19% (9-33) which was driven by high RR: 60% (36-85) & 56% (39-75), respectively, despite alloSCT in first remission. This outcome was not obviously improved compared to UKALLXII (28% and 22%); however, the patient population was older. Patients with KMT2A-AFF1 fusion had OS and RR similar to the small number of patients (n=9) with other KMT2A fusions: 44% (29-58) & 49% (34-65) v 42% (11-71) & 56% (22-93). The outcome of BCR-ABL1 positive patients was not different from the remaining BCP-ALL patients (hazard ratios 0.92 (0.72-1.18), p=0.5 & 0.93 (0.67-1.29), p=0.7).
Additional primary chromosomal abnormalities were detected as follows: ABL-class fusions (ABL1, ABL2, PDGFRB, CSF1R) (n=6, 1.3%), JAK-STAT abnormalities (P2RY8-CRLF2, IGH-CRLF2, JAK2 fusions) (n=34, 1.3%) and ZNF384 fusions (n=12, 3%). Patients with JAK-STAT abnormalities had high rates of MRD positivity post phase 2 induction (76%), high RR (62% (42-82)) and lower OS (35% (18-52)) despite 82% being stratified as high-risk. Three of the six patients with an ABL-class fusion have had an event - 2 early remission deaths and 1 relapse. In contrast, among the 12 patients with a ZNF384 fusion only 2 have relapsed (both after 3 years) and none have died.
Secondary copy number alterations affecting key genes/regions were determined by MLPA in 437 samples. 270 (62%) samples harboured one or more deletion at the following frequencies: IKZF1 (n=169, 39%), CDKN2A/B (n=163, 37%), PAX5 (n=95, 22%), BTG1 (n=48, 11%), ETV6 (n=33, 8%), EBF1 (n=15, 3%), RB1 (n=31, 7%) and PAR1 (n=6, 1%). None of the individual deletions nor the number of deletions were associated with survival, either in the cohort overall or when stratified by BCR-ABL1 status. In particular, IKZF1 deletions had no impact on RR: hazard ratios = 1.04 (0.72-1.49), p=0.850 (Overall); 0.84 (0.45-1.56), p=0.584 (BCR-ABL1); 1.23 (0.51-2.98), p=0.645 (B-Other). In addition, neither of the two recently validated paediatric CNA profiles - UKALL (Blood Advances 2019, 3:148) and IKZF1plus (JCO, 2018, 36:1240) - showed a significant association with outcome in the whole cohort or any relevant subgroup, e.g. BCR-ABL1 or B-other ALL.
Collectively these data indicate that primary chromosomal abnormalities remain stronger prognostic markers in adult ALL than the more recently identified secondary deletions. On the basis of these results, we propose an amendment to the genetic risk classification for adult ALL wherein groups with distinct outcomes (see figure) comprise: (1) very high risk: CK, HoL or JAK-STAT abnormalities; (2) high risk: all KMT2A fusions; (3) Tyrosine kinase sensitive: BCR-ABL1 and ABL-class fusions; (4) low risk ZNF384 fusions; (5) standard risk: all other patients. The integration of these primary genetic risk factors with other risk factor such as age, white cell count and MRD into an overall risk score is a key goal of our current work.
Papaemmanuil:Celgene: Research Funding. Menne:Bayer: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant, Research Funding, Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Astra Zeneca: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Jazz: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant, Research Funding, Speakers Bureau; Kite/Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant, Research Funding, Speakers Bureau; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant, Research Funding, Speakers Bureau; Roche: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Kyowa Kirin: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant, Research Funding, Speakers Bureau; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant; Daiichi Sankyo: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant, Research Funding, Speakers Bureau. McMillan:BMS: Honoraria; Gilead: Honoraria; MSD: Honoraria; Novartis: Honoraria; Sandoz: Honoraria; F. Hoffmann-La Roche Ltd: Honoraria, Speakers Bureau; Pfizer: Honoraria, Research Funding; Celgene: Honoraria, Speakers Bureau. Rowntree:Novartis: Consultancy. Fielding:Novartis: Consultancy; Amgen: Consultancy; Pfizer: Consultancy; Incyte: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal