Introduction: Aggressive B-cell lymphomas can be cured with chemo-immunotherapy; however, those who fail primary therapy and those with indolent lymphomas are rarely curable with such therapy. Novel targeted therapies can disrupt key survival pathways in lymphoma such as regulation of apoptosis (BCL2: venetoclax), B-cell receptor signaling (BTK: ibrutinib), and NFκB survival pathways (IRF4/SPIB: lenalidomide). These agents are active as monotherapy but fail to induce deep responses and require continuous therapy. Also, genetically defined subtypes of lymphoma that best respond to these targeted therapies are undefined. We hypothesized that combining agents that target unique survival pathways in a synergistic fashion will leverage efficacy and time-limited, cyclic dosing will limit toxicities.
Methods: Relapsed/refractory B-cell lymphoma pts, excluding MCL and CLL/SLL, with adequate organ function were eligible. A 3+3 design was used to determine the maximum tolerated dose (MTD) of 4 dose-levels (DLs) of dose-escalated venetoclax (200 mg, 400 mg, 600 mg, and 800 mg) PO D2-14 (starts cycle 2 for DL1) in combination with fixed-dose ibrutinib 560 mg PO D1-14, prednisone 100 mg PO D1-7, obinutuzumab 1000 mg IV D1-2, and lenalidomide 15 mg PO D1-14. Aggressive and indolent expansion cohorts were included at the MTD. Maximum 6 cycles of ViPOR q21 days was given unless PD or unacceptable AE. TLS prophylaxis with IV fluids and allopurinol was given to all pts and VTE prophylaxis and G-CSF use was per investigator discretion. Pre-treatment biopsies were obtained and analyzed for whole-exome sequencing, RNA-sequencing, and copy-number alterations. Baseline CT, PET and BM was performed with CT scans after cycles 1, 2, 4, and 6 and PET after cycle 6 or at time of suspected CR.
Results: 27 pts have been enrolled; 17 in the dose-escalation and 10 in the dose-expansion cohorts. Histologic subtypes include DLBCL (13), FL (8), HGBCL (4), and MZL (2). Median (range) age was 58 yrs (34-77) with stage III/IV disease in 23 (85%), elevated LDH in 20 (74%), and >2 EN sites in 15 (56%) pts. Median (range) of prior therapies was 3 (1-8) and 19 (70%) pts were refractory to last therapy.
A single dose-limiting toxicity (DLT) of G3 intracranial hemorrhage (ICH) occurred at DL1 with concomitant use of enoxaparin and ASA. No other DLTs occurred and venetoclax 800 mg was used in expansion. Heme AEs were most common with >G3 neutropenia, thrombocytopenia, and anemia in 50%, 38%, and 15% of pts and 27%, 16%, and 3% of cycles, respectively. G-CSF was given in 85% of pts in 80% of cycles and no treatment-related febrile neutropenia occurred. Non-heme AEs were mainly G1-2 with rare G3 and no G4-5 events. G3 non-heme AEs included diarrhea (12%), hypophosphatemia and UTI (8% each), and hypokalemia, edema, fever, hypotension, increased AST/ALT/AlkP, a.fib, and ICH (4% each). Dose reductions and delays occurred in 11% and 37% of pts and 5% and 15% of cycles, respectively.
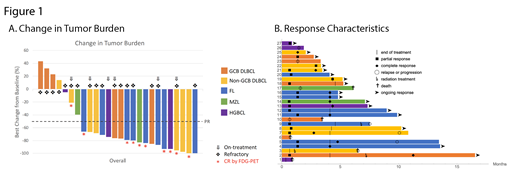
Of 21 pts now off-therapy (14 completed 6C, 4 PD, 3 AE), 20 are evaluable for response with an ORR of 70% (14/20) and 40% (8/20) CR, which occurred across all DLs and NHL subtypes. In 26 evaluable pts overall (6 on active treatment), 85% (22/26) experienced tumor reduction (Fig.1A) with an ORR of 77% (20/26) and 38% (10/26) CR. ORR and CR rate was 69% (11/16) and 25% (4/16) in aggressive and 90% (9/10) and 60% (6/10) in indolent NHL subtypes, respectively. Median TTR and DOR was 1.35 m and not reached, respectively, with 17 (85%) of 20 responses on-going, from 0.16-15.9 m after date of first response (Fig.1B). XRT was given in 1 DLBCL pt with PR to ViPOR who achieved CR and another FL patient with PR and histologic transformation post-therapy as a bridge to CAR-T. One non-GCB DLBCL pt with concurrent sarcoidosis had residual uptake on post-treatment PET and was considered a PR but was MRD negative by ctDNA analysis. With a median potential f/u of 8.5 m, 6-mo PFS and OS was 77% and 87%, respectively.
Conclusions: Combination targeted therapy with ViPOR is safe without TLS or unexpected toxicities observed. Heme AEs, mainly neutropenia, were most common and manageable with G-CSF and no neutropenic fever or severe infections occurred. Early signs of clinical activity, including CRs in refractory pts, are observed with ViPOR and further development plans include phase 1 testing in MCL and phase 2 testing in DLBCL and FL. Updated response durability and molecular correlates of response will be presented at the meeting.
Portell:AbbVie: Research Funding; Pharmacyclics: Consultancy; Janssen: Consultancy; Genentech: Consultancy, Research Funding; Amgen: Consultancy; Bayer: Consultancy; BeiGene: Consultancy, Research Funding; Kite: Consultancy, Research Funding; Acerta/AstraZeneca: Research Funding; TG Therapeutics: Research Funding; Xencor: Research Funding; Roche/Genentech: Research Funding; Infinity: Research Funding. Staudt:Nanostring: Patents & Royalties.
venetoclax, ibrutinib, prednisone, obinutuzumab, and lenalidomide off-label use for relapsed/refractory B-cell lymphomas
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal