Introduction: Limited stage nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) is a highly curable malignancy with an excellent prognosis. Given disease rarity, there are few prospective studies and as a result, diverse treatment approaches are used in both the adult and pediatric populations. At BC Cancer, provincial treatment guidelines for limited stage NLPHL have largely followed that of classical HL: Prior to 2005, radiotherapy (RT) was integrated usually as combined modality therapy (CMT); after 2005, an adaptive approach using 18F-fluoro-2-deoxyglucose positron emission tomography (PET) was adopted. Herein, we evaluated the impact of using this approach.
Methods: Adult (>16 years [y]) patients (pts) diagnosed with limited stage NLPHL (stage 1A, 1B or 2A, non-bulky [<10cm]) from January 1995 to February 2019 were identified in the BC Cancer Lymphoid Cancer Database. Pts were treated based on era-specific guidelines: 1995 to 2005 (CMT era), 2 cycles of ABVD (or ABVD-like chemotherapy [CHT]) and RT, or RT alone in stage 1A high neck node disease; 2005 to present (PET era), 2 cycles of ABVD followed by interim PET (PET2). If PET2 was negative (PETneg), 2 further cycles of ABVD (after 2017, AVD alone) were given; if PET2 was positive (PETpos), RT was administered. PET scans were performed and centrally reviewed at BC Cancer. Prior to 2014, interpretation was based on the International Harmonization Project (IHP) criteria. This was subsequently replaced by the 5-point Deauville (D) scale (PETneg = DX, D1-2, PETpos = D3-5).
Results: A total of 98 pts were identified. Of these, 93 (95%) received active therapy. Patient characteristics did not differ between the two eras: median age 38 y (range 16 - 82 y); male n=73 (74%); stage 2 n=43 (44%); median largest mass size 4 cm (range 2 - 9 cm). In the CMT era (n=37), all pts received active therapy: 84% were treated with ABVD (like) CHT (ABVD n=30 [including ABVD alone n=2], MOPP/ABV n=1); 6 pts with stage 1A received RT alone. In the PET era (n=61), 92% received active therapy (n=56), of which 52 received CHT (ABVD n=49, modified CVPP/ABO with bleomycin omitted n=1, R-CHOP n=2) and 4 pts were treated with RT alone. The remaining 5 pts were observed/refused therapy.
With a median follow up of 7.7 y for all pts (range 0.3 - 20.5 y) (CMT era 13.5 y [3.3 - 20.5 y], PET era 5.5 y [0.3 - 13.5 y]), the time to progression (TTP), progression free survival (PFS), overall survival (OS), and disease specific survival (DSS) at 5 y were 93%, 92%, 98%, and 99%, respectively. There was no difference in outcomes by era comparison (p >0.1) or by stage (1 vs 2) (p=0.93). Overall, there have been 7 lymphoma recurrences (CMT era n=3, PET era n=4), including 3 (3%) with transformed disease (biopsy proven T cell rich B cell lymphoma n=1, presumed aggressive lymphomas based on new splenic nodules n=2).
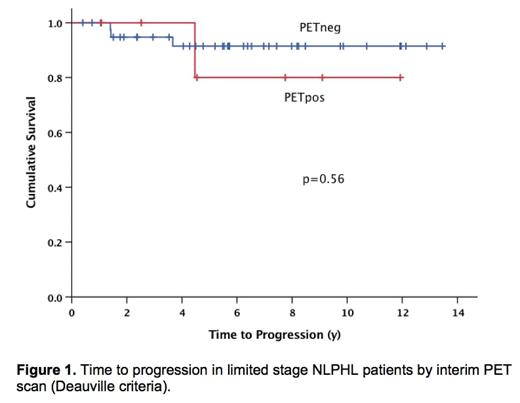
In total, there were 48/52 cases that had a PET2 scan interpreted using the D criteria, including 30 in the IHP time period that were re-reviewed: 85% were PETneg (n=41); 15% were PETpos (n=7). Four CHT treated pts did not receive a PET2 scan: RT added (CHT toxicity) n=3; death (diabetic ketoacidosis [DKA] post cycle 1 ABVD) n=1. All PETpos cases and only 4 PETneg cases (CHT toxicity n=2, PETpos by IHP criteria n=2) received RT. Considering PET-specific outcomes, the 5 y PFS and TTP were both 92% for PETneg and 80% for PETpos cases (p=0.56) (Figure 1). Three recurrences occurred in PETneg pts (DX n=1, D2 n=2), all of which had received ABVD alone but only 1 would have been solely in a RT field. The single recurrence among the PETpos cases (D5) was outside of the RT field.
In the whole cohort, 9 pts have died (CMT era n=5, PET era n=4). Two deaths in the PET era were deemed related to NLPHL: 1 patient refused primary therapy and died of progressive disease and the other died during ABVD of DKA, possibly treatment related. The remaining deaths were due to other malignancies (lung n=2 [one within RT field], vulvar n=1, anaplastic large cell lymphoma n=1) or unknown causes (n=3).
Conclusions: Consistent with other modern series, the outcome of pts with limited stage NLPHL is excellent with both 5 y PFS and OS exceeding 90%. Pts with an interim PETneg scan have a favorable outcome although longer follow-up is needed given the long natural history of NLPHL. This represents the largest experience of a PET-adapted approach in NLPHL and supports that ABVD alone is a viable option in selected patients with consideration of both acute and long term toxicities.
Villa:Roche, Abbvie, Celgene, Seattle Genetics, Lundbeck, AstraZeneca, Nanostring, Janssen, Gilead: Consultancy, Honoraria. Scott:Celgene: Consultancy; Janssen: Consultancy, Research Funding; Roche/Genentech: Research Funding; NanoString: Patents & Royalties: Named inventor on a patent licensed to NanoSting [Institution], Research Funding. Gerrie:Lundbeck, Seattle Genetics: Consultancy, Honoraria. Freeman:Seattle Genetics, Janssen, Amgen, Celgene, Abbvie: Consultancy, Honoraria. Pickles:TarSera: Honoraria, Other: Participated in advisory board meeting; Astellas Inc.: Research Funding; Abbvie, Sanofi: Consultancy, Honoraria. Sehn:Morphosys: Consultancy, Honoraria; TEVA Pharmaceuticals Industries: Consultancy, Honoraria; F. Hoffmann-La Roche/Genentech: Consultancy, Honoraria, Research Funding; F. Hoffmann-La Roche/Genentech: Consultancy, Honoraria, Research Funding; Astra Zeneca: Consultancy, Honoraria; Karyopharm: Consultancy, Honoraria; Merck: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Acerta: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria; Astra Zeneca: Consultancy, Honoraria; TEVA Pharmaceuticals Industries: Consultancy, Honoraria; Lundbeck: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria; Lundbeck: Consultancy, Honoraria; Kite Pharma: Consultancy, Honoraria; Kite Pharma: Consultancy, Honoraria; Acerta: Consultancy, Honoraria; Merck: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; TG Therapeutics: Consultancy, Honoraria; Apobiologix: Consultancy, Honoraria; Morphosys: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; TG Therapeutics: Consultancy, Honoraria; Janssen-Ortho: Honoraria; Janssen-Ortho: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Verastem: Consultancy, Honoraria. Connors:Takeda Pharmaceuticals: Honoraria; Seattle Genetics: Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy. Savage:BMS, Merck, Novartis, Verastem, Abbvie, Servier, and Seattle Genetics: Consultancy, Honoraria; Seattle Genetics, Inc.: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal