Introduction
Indolent lymphomas, such as follicular lymphoma (FL) and marginal zone lymphoma (MZL), are highly radiosensitive and often respond to very low dose radiation therapy (VLDRT). We investigated the outcomes of patients treated with 4 Gy from a large, contemporary, real world cohort, and a subset of potentially curable (PC) patients with early stage (Ann Arbor stage I-II) disease and no prior therapy to the targeted lesion(s) before VLDRT.
Methods
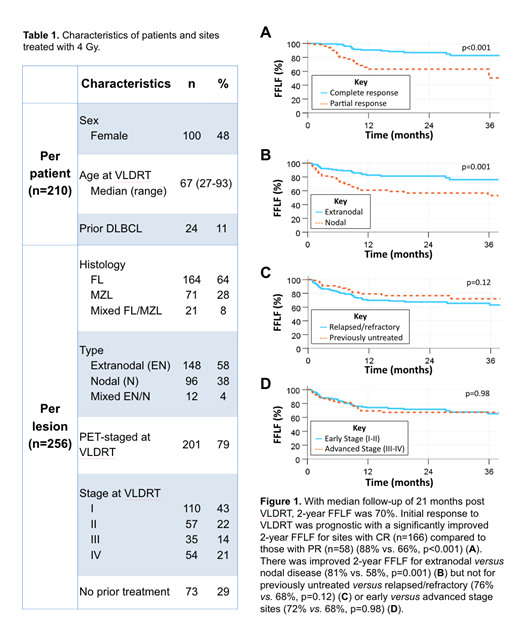
We analyzed 256 treated sites from 210 consecutive adult patients (Table 1) with FL or MZL who were treated with VLDRT of 2 Gy x 2 fractions between 2006 and 2019 at our comprehensive cancer center. Initial overall response rate (ORR) was defined as complete response (CR) or partial response (PR) using Lugano criteria at first follow-up post-RT (median: 2.1 months; Interquartile range: 1.6-2.5 months). Stable disease (SD) or progressive disease (PD) at 2 months post-RT were considered local failure (LF). Freedom from local failure (FFLF) was defined as time from VLDRT to LF. Patients were censored at the start of a subsequent line of therapy if the VLDRT-treated site had not progressed. Event-free survival (EFS) was calculated per patient from VLDRT to LF or distant PD. FFLF and EFS were estimated using Kaplan-Meier and compared using log-rank.
Results
Initial ORR for all sites was 88% (CR: 65%, PR: 23%); 12% (n=31) were initially nonresponding (SD: 7%, PD: 5%). Thirteen sites with initial PR/SD/PD received additional RT (median: 30 Gy) within 6 months of VLDRT and had subsequent CR (n=7), PR (n=5), and PD (n=1). With median follow-up of 21 months, 2-year FFLF was 70%. Initial response to VLDRT was prognostic with a significantly improved 2-year FFLF for sites with CR (n=166) compared to those with PR (n=58) (88% vs. 66%, p<0.001). There was improved 2-year FFLF for extranodal versus nodal disease (81% vs. 58%, p=0.001) but not for previously untreated versus relapsed/refractory (76% vs. 68%, p=0.12) or early versus advanced stage sites (72% vs. 68%, p=0.98).
In the subset of PC patients (n=50), there were 52 lesions. The histology of these sites was split between FL (n=21, 41%), MZL (n=22, 42%) and indolent lymphoma not further classified (n=9, 17%). The majority of the lesions in the PC cohort were extranodal (n=42, 81%). Median follow-up was 1 year with a 1-year EFS of 82%. Of the 12 PC patients who progressed post VLDRT, two thirds developed a distant site of recurrence outside of the VLDRT field. In field recurrence alone was rare (n=4). Diffuse large B cell lymphoma transformation after VLDRT was rare in the PC (n=0) and overall (n=6, 3%) cohort; all cases of transformed DLBCL were diagnosed out of VLDRT field.
Conclusions
Overall, patients with FL and MZL treated with only 4 Gy have excellent initial ORR. Upfront CR is prognostic of improved disease control. Early evaluation following VLDRT identifies nonresponders who may benefit from additional RT and spares many patients from higher doses of RT with durable local control. Our analysis of PC patients suggests that VLDRT does not compromise the standard curative RT approach.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal