Combination Ibrutinib (IB) plus Venetoclax (Ven) for the treatment of Mantle Cell Lymphoma (MCL) has demonstrated efficacy in the relapsed/refractory setting. The AIM trial treated 24 patients with IB monotherapy for 4 weeks (560mg/day) with Ven added (stepwise to 400mg/day) thereafter resulting in an overall response rate of 71% at 16 weeks (Tam et al, NEJM 2018). 5 patients discontinued treatment within 6 months due to resistant disease and 3 patients relapsed. 16 patients remained on treatment for more than 1 year. In this study we examined the longitudinal changes in peripheral blood (PB) immunology in patients treated in the AIM trial in order to identify immunological and inflammatory biomarkers associated with response and to examine if stable control of MCL without further chemotherapy exposure was associated with immunological recovery.
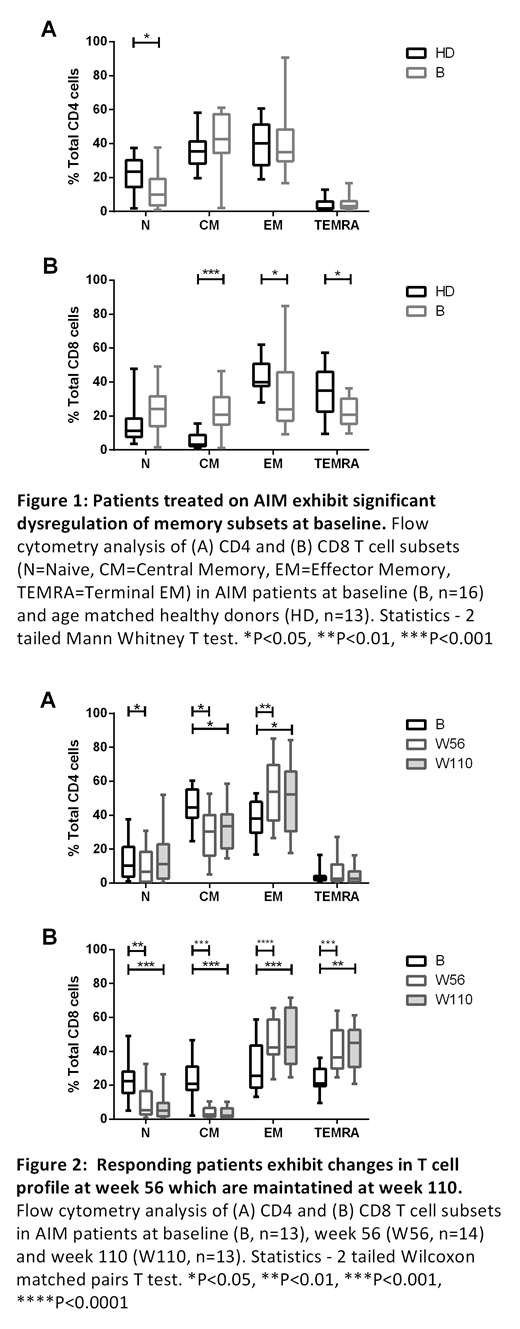
Multiparameter flow cytometry of cryopreserved PBMCs collected at enrolment (baseline), and weeks 4, 16, 56 and 110 of treatment was used to assess the proportions of immune subsets (CD4 and CD8 memory subsets, γδ T cells and CD16+ NK cells) in AIM patients and compared to 13 age matched healthy donor (HD) samples. At baseline samples from MCL patients exhibited alterations in multiple immune subsets - most notably skewing in CD8+ memory subsets (Figure 1). Despite reduction of circulating B cell numbers consistent with clinical responses, there were no significant changes to PB immune subset distributions between baseline and 16 weeks. However at the later time points of 56 and 110 weeks there was evidence in responding patients of PB immunology normalisation to HD levels in T cell subsets including a shift in CD8 T cells from Naïve and Central Memory (CM) to Effector Memory (EM) and Terminally differentiated EM (TEMRA) phenotype and a shift in CD4 T cells from Naïve and CM to EM phenotype (Figure 2). Increased proportions of γδ T cells (Baseline 2.8 ± 3.0% week 56 4.4 ± 3.4% P<0.05) and CD16+ NK cells (Baseline 40.1 ± 28.0% week 56 79.1 ± 21.0% P<0.01) were also observed.
T cell function assessed by intracellular IFNγ, TNFα and IL-2 in CD4 and CD8 T cells in response to T cell stimulation beads showed no change in IFNγ or TNFα production by CD4 or CD8 cells following therapy. In patients with elevated IL2+ CD4 and CD8 populations at early time points, these normalised by week 56 to HD levels.
To further examine changes in immune function pathways, targeted multiplex gene expression profiling using 770 gene NanoString nCounter® PanCancer Immune Profiling Panel was performed on PBMCs at baseline and weeks 4, 16 and 56 and analyzed using nSolver advanced analysis module. Consistent with the flow cytometric findings there were minimal changes in gene expression at week 16 compared to baseline. The greatest changes were observed at week 56 with alterations in multiple pathways including increased signalling through complement, adhesion, TNF superfamily and transporter pathways in responding patients. The top upregulated genes at week 56 were CTSS (Cathepsin S), FCER1G (Fc fragment of IgE), S100A8 (S100 calcium binding protein A8) and CD14 while the top downregulated gene was CD22 (reflecting the change in B cell burden). Increased expression of C1QA and C1QB at week 16 was significantly associated with disease non-response or relapse on IB + Ven and warrants further investigation in an independent cohort to assess its applicability as a predicative biomarker for patient response.
Our findings show that long term treatment with combination IB and Ven in MCL is associated with immune recovery and changes in the expression of inflammatory biomarkers. This study demonstrates that while short term assessments can be used to examine clinical disease responses, long term assessments are required to determine the immunological consequences of small molecule inhibitors. Restoration of immune system function in these patients may allow responses to subsequent immunotherapies and suggests that, in contrast to conventional chemotherapy-based regimens, this combination targeted therapy may result in beneficial impacts on immunological recovery.
Handunnetti:Gilead: Honoraria. Anderson:Walter and Eliza Hall Institute: Employment, Patents & Royalties: Institute receives royalties for venetoclax, and I receive a fraction of these.. Roberts:AbbVie: Other: Unremunerated speaker for AbbVie, Research Funding; BeiGene: Research Funding; Janssen: Research Funding; Walter and Eliza Hall Institute: Patents & Royalties: Institute receives royalties for venetoclax, and I receive a fraction of these.; Australasian Leukaemia and Lymphoma Group: Membership on an entity's Board of Directors or advisory committees. Seymour:AbbVie: Consultancy, Honoraria, Research Funding, Speakers Bureau; Janssen: Consultancy, Research Funding; Roche: Consultancy, Research Funding, Speakers Bureau; Acerta: Consultancy; Celgene: Consultancy, Research Funding, Speakers Bureau; Takeda: Consultancy. Tam:Janssen: Honoraria, Research Funding; Pharmacyclics LLC, an AbbVie company: Honoraria; Roche: Honoraria; AbbVie: Honoraria, Research Funding; BeiGene: Honoraria; Novartis: Honoraria. Ritchie:Sanofi: Honoraria; Novartis: Honoraria; Imago: Research Funding; Beigene: Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy; BMS: Research Funding; Takeda: Research Funding. Koldej:NanoString Technologies: Other: Travel grant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal