Introduction
Interactions between tumor cells and the immune system play a critical role in regulating tumor development. Immune-based therapies have shown variable responses in diffuse large B-cell lymphoma (DLBCL) which suggests that the immune cell composition of the tumor microenvironment (TME) influences response to these agents. However, the key determinants of the immune TME are poorly understood. We have recently shown that indolent lymphomas can be stratified as immunologically 'hot' or 'cold' (Tobin et al J. Clin Oncol, in press) and sought to test for this in DLBCL. Also, given that beta-2-microglobulin (B2M) has a key role in antigen presentation and its loss is a frequent immune evasion mechanism in DLBCL, we determined the effect of B2M expression on the nature and magnitude of immune infiltration in the tumor microenvironment of DLBCL.
Methods
Ninety-seven de novo systemic DLBCL FFPE biopsies underwent targeted exon re-sequencing of B2M (Illumina) in addition to quantitative gene expression of Β2M, immune effector (CD4, CD8, CD56, CD137), immunosuppressive macrophage markers (CD68, CD163) and immune checkpoints (TIM3, LAG3, PD1 and PDL1) (Nanostring Technologies). B2M promoter methylation by mass array, immunohistochemistry for the above markers and high throughput T-cell receptor β sequencing (Adaptive Biotechnologies) were performed on a subset of cases. Genomic findings were validated in a whole exome and transcriptome cohort of approximately 1000 DLBCL samples (Reddy et al Cell 2017).
Results
Β2MMut were detected in 14/97 (14.4%) samples and had lower Β2M gene expression compared to Β2MWT (p = 0.0094) and all of these showed B2M protein loss. However, 29/40 (72%) of B2MWT samples tested also had B2M protein loss. There was no differential methylation of B2M promoter regions observed compared to lymph node controls. Results indicate that mechanisms other than mutation and methylation status contribute to loss of B2M surface expression and that a more comprehensive assessment of B2M expression within tumor tissues is achieved by B2M digital gene quantification.
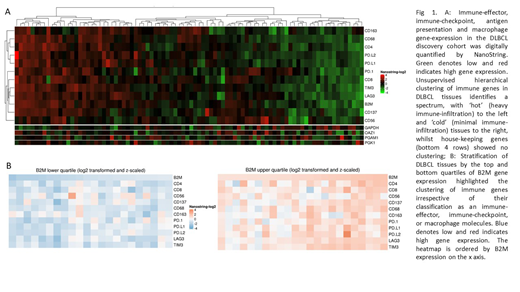
Consistent with this, there were no significant differences in expression of intra-tumoral immune markers between B2MMut and B2MWT tissues, whereas gene expression of B2M was significantly associated and positively correlated with the gene expression of CD4, CD8, CD56, CD137, CD68, CD163, PD1, PDL1, LAG3 and TIM3 (all p <0.01) and with the protein expression of CD8, CD56, CD137, PDL1 and LAG3 (all p <0.01), irrespective of their classification as an immune-effector, immune-checkpoint or macrophage markers. These observations are consistent with a co-ordinately regulated immune response, indicating an adaptive immune-checkpoint response to regulate immune-effector activation. In keeping with this, the housekeeper genes did not correlate with immune gene expression indicating that high or low co-ordinate expression of immune genes was not reflecting tissue RNA quality or quantity (Fig 1).
Next, we tested the discovery cohort for relationships with the TCR repertoire. High B2M gene expression was significantly associated with reduced TCR diversity (p = 0.0101) compared to low B2M gene expression, suggesting that clonal T cell expansions are more likely with intact antigen presentation. The validation cohort also demonstrated that B2M gene expression correlated with immune cell infiltration and additionally showed that B2M positively correlated with the gene expression of HLA Class I//II molecules and a range of regulatory, transport and assembly molecules involved in the antigen presentation machinery pathway. However, no differential survival benefit was observed in patients with high versus low B2M.
Conclusions
In summary, digital gene expression is a robust measure of B2M quantification in the TME. Our data show that high B2M gene expression reflects an immunologically active or 'hot' tumor microenvironment in DLBCL characterised by higher levels of immune cell infiltration. These findings indicate that B2M gene expression level could be used as a biomarker of an active intra-tumoral immune response in DLBCL. Further studies are required to determine if B2M gene expression may have a role in stratifying the selection of patients in whom immune-based therapies are more likely to be effective.
Gould:NovoNordisk: Other: Travel funding - domestic flights to attend education, May 2018. Keane:MSD: Consultancy; BMS: Research Funding; Celgene: Consultancy; Gilead: Consultancy; Roche: Consultancy, Other: Travel Grant. Hertzberg:Takeda: Consultancy, Honoraria; MSD: Consultancy; Roche: Consultancy, Honoraria. Gandhi:Gilead: Honoraria, Research Funding; Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche: Honoraria, Other: Travel Support; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Merck: Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal