Background: Acute myeloid leukemia (AML) is an aggressive hematological disease. Allogeneic hematopoietic stem cell transplantation (Allo-HSCT) and chemotherapy are major treatment regimens for AML. However, prognostic markers cannot guide the decision for a specific treatment, as they are related with a various prognosis regardless of the given treatment. HOXA (homeobox A) genes cluster could promote tumor survival, proliferation, invasion, and increase the resistance of AML. The aim of this study was to screen potential miRNAs (microRNAs) that would target HOXA genes, and evaluate the utility of miRNAs in AML, help patients choose a better treatment between chemotherapy and allo-HCST.
Methods: Clinical data and RNA-Seq expression data of selected cases were provided by The Cancer Genome Atlas (TCGA). Genome-wide screening was performed to identify miRNA in a heterogeneous AML population. Univariable Cox proportional hazards models and Multivariable Cox proportional hazards models were employed to identify whether OS and EFS would be affected by other variables.
Results: In this study, totally 162 AML patients were recruited. All patients were firstly divided into the chemotherapy and allo-HSCT groups. Subsequently, according to median values of miR-340, patients were divided into miR-340high and miR-340low expressers, respectively. In chemotherapy group, no difference was found in clinical characteristics, such as the median age, FAB subtypes, karyotypes and genes mutation between miR-340high and miR-340low expressers. However, miR-340low expressers often accompanied with high first relapse rate or death rate in one year than high expressers (P=0.012; 82.2% vs 55.6%).
To identify the independent prognostic role of miR-340 in chemotherapy group patients, Univariable and Multivariable Cox proportional hazards models were performed. We found that miR-340lowpatients showed shorter OS (P=0.0005; 5-year OS, 35.6% vs. 5.4%) and EFS (P=0.0005) compared with high expressers. In multivariable analysis, miR-340low patients showed reduced OS (P=0.004; HR: 2.07) and EFS (P=0.01; HR: 1.909) after adjusting other co-variates, such as age, WBC count and several genes mutation in chemotherapy group. Therefore, low miR-340 amounts could be an independent adverse bio-marker in AML patients undergoing chemotherapy. However, in the allo-HSCT group, miR-340 expression level was not associated with outcome in AML patients.
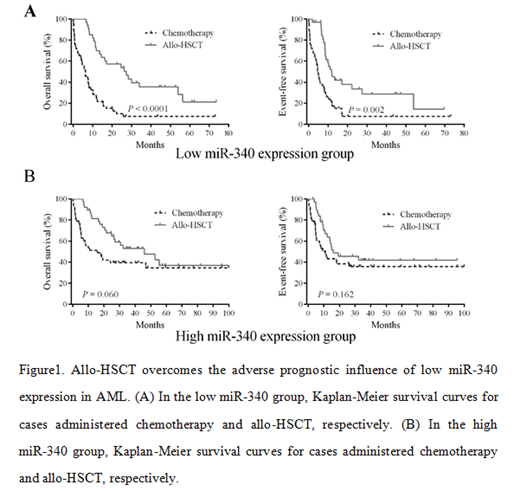
To further explore the potential of allo-HSCT in overcoming the adverse characteristics of low miR-340 amounts, the whole 162 patients were regrouped into miR-340low and miR-340high groups. Then patients were divided into chemotherapy and allo-HSCT subgroups. Subgroup analysis revealed that miR-340low patients had significantly longer OS (P<0.0001; HR: 0.316; 95%CI: 0.167-0.459) and EFS (P=0.002; HR: 0.391; 95%CI: 0.231-0.622) in allo-HSCT subgroup than in chemotherapy subgroup (Figure 1). However, in cases highly expressing miR-340, no difference in survival events was detected between the two treatment subgroups. These findings indicated, allo-HSCT may overcome the adverse prognostic effects of low mir-340 expression. Therefore, for low miR-340 cases, early allo-HSCT may be a better option.
To explore underlying biological functions of miR-340, we examined gene expression signatures related to the miR-340 expression in AML patients. We observed 135 genes expression levels that associated with miR-340 expression, with 61 and 74 showing positive and negative correlations, respectively. Gene Ontology showed that these genes involved in cellular and developmental processes, transcription regulation, immune system process, cell apoptosis and proliferation, myeloid cell differentiation and hematopoietic organ development. Furthermore, miR-340 expression was negatively correlated with HOXA and HOXB cluster levels. Strikingly, HOXA10, HOXB2, MEIS1 and PRDM16 were predicted miR-340 targets according to in silico analysis. The results hint a prospective regulatory mechanism that links miR-340 to HOXA genes associated with AML.
Conclusions: Our data indicate that decreased miR-340 expression predicts an adverse prognosis and allo-HSCT may overcome the potential adverse characteristics of low miR-340 expression. Therefore, lower miR-340 cases should be strongly considered for early allo-HSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal