
Background:
Literature on Acute Myeloid Leukemia (AML) survival and prognostic factors were often derived from strict trial studies from developed country. A simple yet practical prognosis index has not been developed and tested in resource limited setting such as Malaysia. We described the treatment outcome and designed a 10 point prognostic index to predict survival of adult AML (non-M3) in real clinical practice in Malaysia.
Methods:
Data were retrospectively collected and analyzed from all adults with AML diagnosed and treated from 2007 to 2017 in three main hematology centers in Malaysia, Ampang Hospital, Sarawak General Hospital and Miri General Hospital. Treatment pattern and survival outcome were described. Multivariable analysis using Cox regression statistics were performed to identify significant prognostic variables affecting overall survival. Each variable were assigned points based on hazard ratios. A sum of the points led to a maximum score of 10. Patients were then categorized into low (0 point), intermediate (1 to 3 points) or high-risk group (4 points or above).
Results:
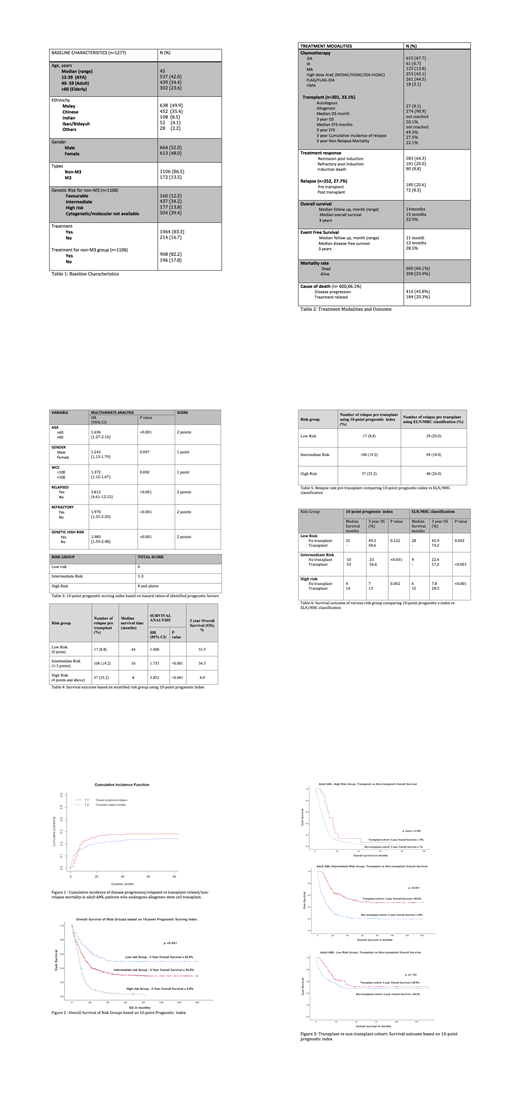
Demographics and treatment outcome of patients are shown in Table 1 & 2. There were 1277 adult patients, diagnosed with AML where 86.5% (n= 1106) of them were non M3 AML. Out of these, 908 patients (82.2%) received intensive chemotherapy treatment. Median age of diagnosis was 45 years. The remission post induction rate was 64.3% with induction death, refractory and relapse rate of 8.8%, 20.0% and 27.7% respectively. Median overall survival (OS) and Event Free Survival (EFS) time was 15 months and 12 months. The 3-year OS and EFS was 32.9% and 28.5% respectively. At the time of analysis, 66.1% of patients were dead (n=600) with disease progression being the main cause of death (n=416, 45.8%). Three year overall OS for patients who underwent allogeneic stem cell transplant (n=301, 33.1%) versus patients without transplantation were 53.7 % versus 22.0 % (HR 2.597, p <0.001). Cumulative incidence of relapsed and non-relapse mortality for transplant patients, shown in Figure 1 were 27.5% and 22.1%.
Multivariate analysis in Table 3 showed that age 60 years old and above, male gender, white cell count more than 100 x 109 /L ,relapsed less than 12 months of treatment, refractory state after induction and high risk genetic group (based on EuropeanLeukemiaNet/Medical Research Council risk stratification by genetics) are prognostic factors associated with worse OS and EFS.
The information was used to develop a 10 point prognostic index based on calculation described in Table 3. Overall survival decreased with each additional index point. When stratified according to risk group, the 3 year OS for low risk, intermediate risk and high risk group was 53.3%, 34.3% and 4.9% respectively. This is shown in Table 4 & Figure 2. Relapse rate was also lower in the low-risk group (8.8%), compared to intermediate-risk group (19.2%) and high-risk group (35.2%). Comparing transplant and non transplant cohort shown in Figure 3, there was no survival benefit in the low-risk group (58.6% vs 49.2%, p=0.122) but significant survival benefit in both intermediate-risk group (56.6% vs 23%, p<0.001) and adverse-risk group (13% vs 7%, p=0.002).
Discussion/Conclusion:
This is one of few survival studies that involved patients of different ethic groups in Asia (Malay, Chinese, Indian and native Borneo Sarawakians). Our results are comparable to data from large population based database such as US SEER and EURO CARE. This is the first prognostic index incorporating genetics, baseline characteristics and dynamic response, eg. refractory and/or relapsed post induction in non M3 AML. The results reaffirmed the importance of these factors in determining the clinical outcome and prognosis of patients with AML. When stratified using our 10 point prognostic index, our cohort of patients who is in low risk group has lower relapse rate and did not have significant survival benefit from allogeneic transplant compare to stratification using only the ELN/MRC genetic classification.(Table 5 & 6). In resource limited setting, measurable residual disease (MRD) monitoring and advanced genetic testing are difficult financially. This prognostic scoring index is an economical and practical alternative to guide physicians on treatment after induction therapy. However, it still needs to be validated by a larger cohort of patients in a prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal