Background
North Middlesex University Hospital (NMUH) is a 400 bed acute hospital in London, United Kingdom. The hospital is a specialist centre for the treatment of inherited red cell disorders caring for approximately 500 adult patients with Sickle Cell Anaemia (SCA) and performing a large number of emergency and elective blood transfusions including automated exchange transfusions, which are an increasingly important cornerstone in the treatment of SCA.
In order to minimise risks of allo-immunisation, international guidelines recommend that sickle cell patients are fully phenotyped prior to first transfusion and receive red cell units that are ABO, Rh (DCcEe) and K matched. This has been implemented at NMUH since the 1990s. However, there is concern that the rate of generation of allo-antibodies is still significant.
Methods
NMUH undertook a retrospective cross-sectional survey of all currently registered adult (>18 years old) patients with haemoglobin genotypes SS and SC, using local transfusion records dating back to 1991. The Laboratory Information Management System (LIMS) was interrogated to provide the current antibody status of each patient as well as the number of red cells received. To account for transfusions before 1991, outpatient annual review data was examined where numbers of units transfused were recorded. Multivariate logistic regression models were used to explore the relationship between the presence of allo-antibodies and the following variables: sex, age, genotype, cumulative number of transfusions and pregnancy.
Results
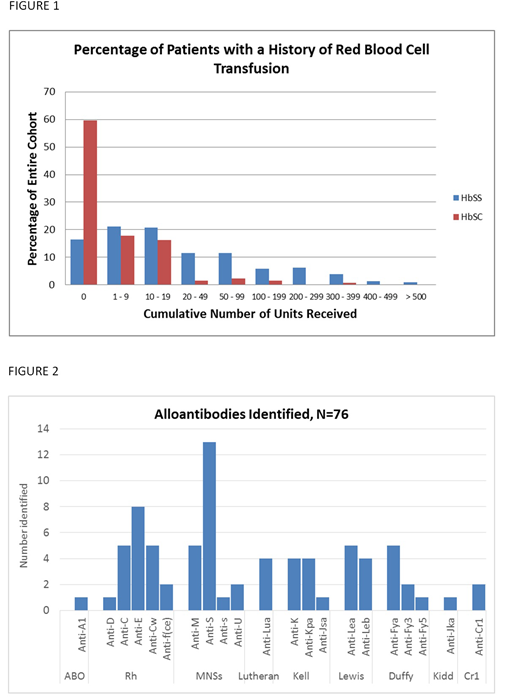
A total of 336 patients with HbSS (n=207) and HbSC (n=129) were identified. The mean age was 39. Male to female split was 43% to 57%. In the HbSS group, 73% (n=173) had received at least one blood transfusion. This was 40% (n=52) in the HbSC group. Number of units received ranged from 1 to greater than 500 for those on regular exchange programmes. An estimate of the number of cumulative red cell units given is shown in Figure 1. 18% (n=42) of transfused patients had alloantibodies ranging from 1 (50% of patients) to a maximum of 5 antibodies). 79% (n=33) of those with allo-antibodies were female.
76 antibodies were identified in total and the breakdown of antibody frequency is shown in Figure 2. 38% (n=29) of antibodies were directed against antigens of the MNSs/Fy system and 33% (n=25) were Rh and /K directed. Multivariable regression showed female sex (OR = 3.54; CI 1.55 - 9.00), age (OR = 1.03; CI 1.00 - 1.05) and number of units transfused (OR = 1.40; CI 1.18 - 1.65) were all independent predictors for antibody formation (p<0.05). Subgroup regression analysis of the female patients showed no impact of pregnancy (p>0.05).
Conclusion
We presented retrospective data from a large cohort of patients with SCA. Limitations included the fact that transfusions prior to 1991 could not be retrieved from the LIMS and were recorded based on annual review data, which although comprehensive, cannot guarantee to fully account for transfusions received elsewhere. The data suggests that despite transfusing in accordance with international guidelines, the level of allo-immunisation remains significant and is particularly marked in females. The majority consisted of potentially hazardous antibodies (Rh/K/Ss/Fy), with only 18% being of limited clinical importance (M/Le). The relatively high frequency of anti-Rh/K requires further investigation to ascertain if these are due to phenotype/genotype mismatch or due to transfusion of inappropriate units at other centres. The high incidence of Ss/Fy antibodies is in line with findings from other papers [Compernolle et al, Transfusion 2018;58;1555-1566] and warrants further research into selecting Ss/Fy compatible units, especially in the younger generation of SCA patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal