Introduction:
An estimated 16% of acutely ill medical patients are at risk of developing venous thromboembolism (VTE) in the absence of appropriate VTE prophylaxis. Hence, the appropriate use of risk stratification models such as Padua Prediction Score(PPS) and prophylactic agents is paramount to mitigate the risk of VTE among hospitalized patients. Despite the existence of VTE prophylaxis guidelines published by the American Society of Hematology(ASH), the risk stratification models and VTE prophylactic agents are often either over- or under-utilized by the clinicians.
Objective:
To determine the characteristics of VTE prophylaxis orders in a community hospital and the rate of PPS utilization by the clinicians in assessing the VTE risk. The secondary outcome is the appropriateness of the prophylactic agent prescribed based on the patients' risk stratification.
Method:
We conducted a retrospective chart review of 480 hospitalized medical patients for the month of September 2018. We assessed the adherence of our clinicians to the use of PPS and the VTE prophylaxis agents used per the ASH 2018 VTE Guidelines. Inclusion criteria: ≥18-year-old patients admitted to medical service. Exclusion criteria: admission to non-medical services or ICU, on-going anticoagulation therapy, and pregnancy. Statistical analysis was performed to compare the use of VTE prophylactic agents between teaching and non-teaching services. A survey consisting of 9 questions was distributed to 15 resident physicians to assess their understanding of the VTE prophylaxis for hospitalized medical patients per the ASH 2018 recommendations.
Results:
Based on our inclusion criteria, a total of 333 patients were eligible for data analysis. Only 3.3%(11/333 patients) had a PPS documented. We re-calculated the PPS for the missing data, 222 patients had a PPS of <4 and 111 patients had a PPS of ≥4.
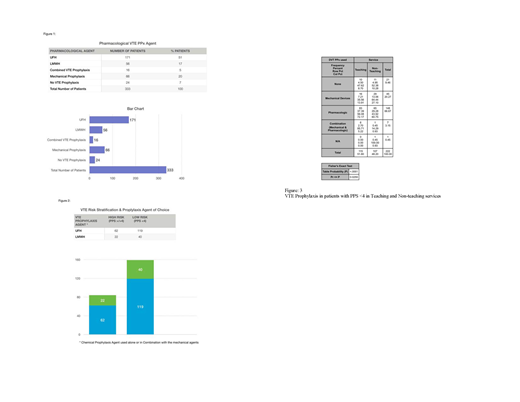
Out of 333 patients, 243 of the patients received chemical prophylaxis either alone or in combination with a mechanical agent, 66 of the patients received mechanical prophylaxis, and 24 of the patients received no VTE prophylaxis (Fig.1). No VTE or bleeding events were recorded in any of our patients. Majority of the patients, 70.37% were prescribed unfractionated heparin(UFH), 23.04% received low molecular weight heparin(LMWH), 6.5% received a combined VTE prophylaxis (Fig.1).
Notably, 71.62% (159/222) low-risk for VTE (PPS <4) patients were prescribed chemical VTE prophylactic agents either alone or in combination with the mechanical agents (Fig.2). The extra expense incurred secondary to unnecessary chemical prophylaxis for low-risk patients was calculated about $18/patient (based on an average length of stay of 5 days and cost of UFH dosed thrice daily for a total of 15 vials/patient). In our study, expenditure on these 159 patients amounts to $2862/month, and a calculated approximate annual expenditure of $34,000/year.
Based on Fisher's exact test there was a statistically significant difference between the teaching and non-teaching services in prescribing VTE prophylactic agents [p=0.026] among patients with PPS<4. The non-teaching service clinicians were less likely to prescribe pharmacologic VTE prophylaxis compared to teaching clinicians [60.75% vs. 72.17%] (Fig.3). Nonetheless, there was no statistical significance between the two services in the use of VTE prophylactic agent in patients with PPS ≥4 [p=0.38].
Our resident survey revealed that 60% of the residents used their clinical judgment for initiating VTE prophylaxis and did not utilize PPS. 80% of them were aware of the ASH panel 2018 guidelines about LMWH being the VTE prophylaxis agent of choice.
Conclusion:
Our study revealed that PPS remained underused among the clinicians in our community hospital before prescribing VTE prophylactic agent. The selection of appropriate VTE prophylactic agent remained underscored among our clinicians. It was notable that UFH continued to be the most commonly prescribed VTE prophylactic agent among hospitalized medical patients in our hospital. As a result, we are determined to educate, improve, and raise awareness on the use of PPS and prophylactic agent among our clinicians in accordance with the ASH 2018 VTE guidelines.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal