Introduction:
Antiphospholipid syndrome (APS) is an autoimmune disorder caused by "antiphospholipid" antibodies (aPL) directed in part against β2-glycoprotein I (β2GPI). Though β2GPI is proposed to have numerous anti- and procoagulant properties in vitro, its effect in vivo is not well studied. Β2GPI binds thrombin via exosite 1 and exosite 2 and impairs thrombin activity, in particular thrombin-mediated activation of FXI. Β2GPI also is found to inhibit thrombin mediated platelet aggregation and it inhibits phospholipid-dependent coagulation reactions, such as the prothrombinase and tenase complexes. β2GPI also may inhibit the activation of protein C, an effect potentiated by antiphospholipid antibodies. However, there is little direct information on β2GPI effects on thrombosis in vivo.
Methods:
We created β2GPI deficient mice using CRISPR-Cas9 technology. Two pairs of guide RNAs (sgRNAs) flanking upstream and downstream exons 2 and 3 on a C57BL/6J background were designed using the CRISPOR program (http://crispor.tefor.net/crispor.py). The PCR product spanning exons 2 and 3 was used to test the efficiency of SgRNA cleavage using the Guide-it Complete sgRNA Screening System. An efficient pair of sgRNAs, one upstream of exon-2 (sgRNA-UP: ATCTTTCCCTTATATGCTAG) and another downstream of exon-3 (sgRNA-DOWN: TCGAGTTAATCACGTGTAGG) were injected into the embryos of C57BL/6J mice with Cas9 protein. Founder mice were genotyped to identify mice with expected deletions in the APOH (encoding β2GPI) gene. Strong founder male mice containing mutated APOH were crossed with wild type C57BL/6J females. Male and female F1 heterozygotes were backcrossed and F2 homozygous knockouts (APOH-/-) were characterized.
The Rose-Bengal carotid artery thrombosis assay was performed on 6 to 9 week old wild type and APOH-/- mice. In brief, mice were anesthetized using sodium pentobarbital intraperitoneally. Rose Bengal [isobenzofuran-1(3H)9[9H] xanthan)-3:1 dipotassium salt] was injected via tail vein at a concentration of 50 mg/kg in 0.9% saline in a 100 μl volume. Green laser light at 540 nm was applied to the carotid artery following injection of Rose Bengal. Continuous flow was monitored at the site of injury and time to occlusion was determined.
Results:
Genotyping of APOH-/- mice revealed complete deletion of exon 2 and 3 (1900 to 2000 bp deletion). Plasma derived from WT-mice, APOH+/- and APOH-/- mice was analyzed by immunoblotting: APOH-/- mice lacked β2GPI protein while heterozygotes had intermediate levels. APOH-/- mice appeared healthy with no obvious phenotype.
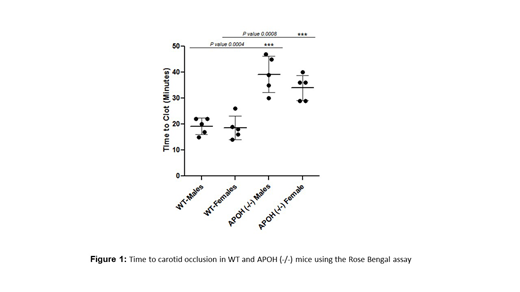
Carotid artery occlusion times were compared in 5 WT and 5 APOH-/- male mice. In WT-mice, complete vessel occlusion occurred at a mean time of 19.2 +/- 3.1 min, whereas the occlusion time in APOH-/- mice was prolonged approximately 2-fold (38.6 +/- 7.1 min). The prolonged time to occlusion in APOH-/- mice was highly significant (p <0.0005).
Conclusion:
These results indicate that APOH-/- mice have a net anticoagulant phenotype compared to WT mice, and suggest that β2GPI may have procoagulant properties in vivo. The mechanisms underlying this observation are not immediately apparent and are currently under investigation. However, given the reported effects of β2GPI on inhibition of thrombin generation and thrombin-mediated platelet activation, these findings are unexpected. Additional studies with other thrombosis models are in progress. Identification of β2GPI as a "procoagulant protein" suggests a reconsideration of its role in the pathogenesis of antiphospholipid syndrome.
McCrae:Sanofi Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Pfizer Pharmaceutical: Membership on an entity's Board of Directors or advisory committees; Rigel Pharmaceutical: Membership on an entity's Board of Directors or advisory committees; Dova Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal