Background: Thrombotic microangiopathy (TMA) has myriad causes with only subtle differences at presentation. Thrombotic thrombocytopenic purpura is one of the etiologies, and traditional teaching is that initiation of treatment with plasmapheresis (PLEX) is time sensitive allowing mitigation of the otherwise high morbidity and mortality of this condition. If TTP is suspected, PLEX is frequently initiated prior to availability of confirmatory lab tests. In contradiction to this, a recent publication by Liu et al (Blood 2017) found that early initiation of PLEX was not associated with improved inpatient mortality. We aim to study inpatient outcomes and predictors of early initiation of PLEX in this population.
Methods: This is a retrospective cohort analysis of NIS database (year 2016). Our cohort of interest was adult patients with TMA who underwent plasmapheresis and we identified them by selecting those ≥18 years of age, with ICD-10-CM diagnosis code of TMA and procedure code for PLEX. Early PLEX was defined as initiation of PLEX within 24 hrs of admission and late PLEX as beyond 24 hrs. Primary outcome was inpatient mortality and secondary outcomes were length of stay (LOS), predictors of early initiation of PLEX and mean total charge (TOTCHG). Associated factors were analyzed using a multivariate regression model. We used STATA for statistical analysis.
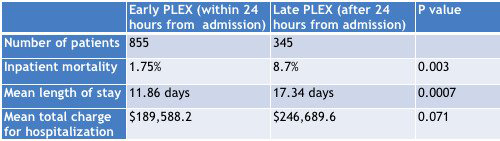
Results: A total of 2064 admissions with thrombotic microangiopathies (TMA) were identified in 2016, of which 1200 (58.1%) received PLEX. Death in the same admission occurred in 120 (5.8%) of all TMA patients, but only in 45 (3.75%) of those who underwent PLEX. Among those who received PLEX for TMA, mean age was 49.2 years, 71.25% (n=855) had early PLEX, 70.4% were female, 38.75% Caucasian and 38.3% African American. The mean time to initiation of PLEX was 2.01 days. Within the cohort of those who received PLEX, inpatient mortality was lower in those with early initiation of PLEX (OR 0.13, p 0.005) and higher with increasing age (OR 1.10, p 0.006) after adjusting for gender and all hospital characteristics (geographical location, urban or rural location of hospital, hospital teaching status, size). LOS was shorter in early PLEX vs late PLEX (by 5.25 days, p 0.0001) and was longer in those admitted to a teaching hospital vs non teaching hospital (by 3.08 days, p 0.038) keeping income quartile of patient's address, gender, Charlson Comorbidity Index (CCI) and other hospital characteristics constant. Likelihood of receiving PLEX within 24 hours of admission was lower in those who were admitted over the weekend (OR 0.36, p 0.006) after adjusting for other factors. There was no association of early initiation of PLEX with age, gender, race, CCI, mean income quartile for patient's address, insurance status, hospital region, urban or rural location of hospital, hospital teaching status. Total charge was approximately $54,759 higher (with a trend to significance, p=0.054) for those receiving late PLEX versus early PLEX after adjusting for patient demographics and hospital characteristics.
Conclusion: Among patients admitted with TMA, inpatient mortality, length of stay and mean total charge for hospitalization was lower in those who had initiation of plasmapheresis within 24 hours of admission. Admissions over weekends were associated with lower likelihood of early initiation of PLEX. Given the better inpatient outcomes with early initiation of PLEX, this should be an area of quality improvement interventions in the future.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal