Background. Neutrophil Extracellular Traps (NETs) are composed of extracellular decondensed chromatin networks that play an important role in immune and inflammatory response regulation. Simple and reliable identification of NETs has been challenging. Automated analyzers such as the CellaVision® Hematology Autoanalyzer identify a subset of cell-derived entities as smudge cells. We hypothesize that, in addition to the typical degenerated lymphocytes (DLs) forming smudge cells, a proportion of smudge cells as identified by the Autoanalyzer are actually NETs. Since patients with high numbers of NETs have increased and specific morbidities, accurate and rapid identification of NETs may be clinically useful.
Methods. To test our hypothesis, we analyzed peripheral blood smears from samples processed by the CellaVision® Hematology Autoanalyzer. To differentiate NETs from DLs we used morphologic characteristics, immunohistochemistry, and flow cytometry. After immunohistochemistry and flow cytometry informed our morphologic classification of NETs and DLs, we relied solely on morphology. Smears with >20% smudge cells were classified as the study group; the control group had < 5% smudge cells. Medical chart review was performed by investigators blinded to sample group designation. Data obtained from chart review included patient demographics; presence of bacterial and/or viral infection occurring <1 week of sample collection; myeloproliferative and lymphoproliferative disorders (LPD); solid organ malignancy and/or transplant; sickle cell disease; chronic kidney (CKD) and liver diseases; autoimmune disorders; HIV; thrombotic events. We reviewed the same sample laboratory data for hemoglobin, platelet counts, and white blood cell (WBC) counts. Statistical analyses were performed using two-sided t-test with α =0.05 for continuous variables, chi-square for categorical variables with samples size >10 and Fisher's exact tests for categorical variables with sample size <10.
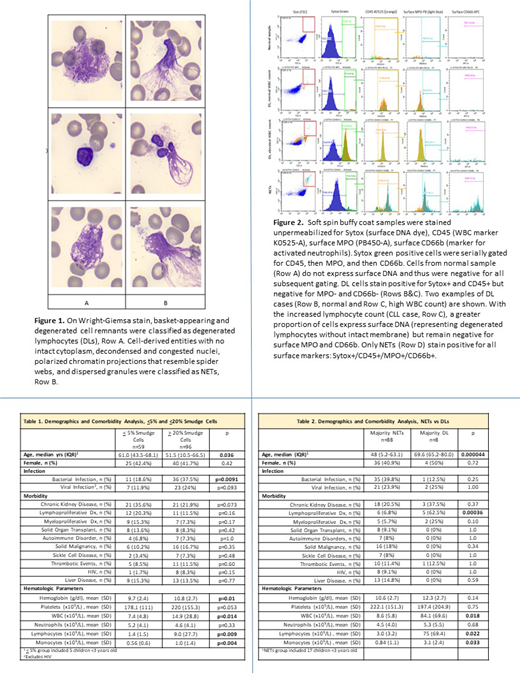
Results. 155 samples were used in the analysis: 96 in the study group, 59 in the control group. Cell-derived entities staining strongly with myeloperoxidase (MPO), neutrophil elastase (NE), and leukocyte alkaline phosphatase (LAP) were classified as NETs. On flow cytometry, these NETs are at least twice as large as WBCs, display extracellular DNA (as identified by Sytox dye) and stain positively for MPO [Figure 1]. On Wright-Giemsa stain, these appeared morphologically as cell remnants with decondensed nuclei, no intact cytoplasm, dispersed granules, and polarized chromatin projections that resemble spider webs [Figure 2]. Of 96 patient samples with >20% smudge cells, morphologic analyses designated 88 as NETs and only 8 as DLs.
Comparing patients with >20% to <5% total smudge cells, the former had a higher incidence of bacterial infections (p=0.0091), as well as higher WBC, lymphocyte, monocyte counts and hemoglobin (p=0.014, 0.009, 0.004, 0.01 respectively) [Table 1]. High percentage of smudge cells correlated with a higher percentage of bacterial infection when compared to those with fewer smudge cells despite a non-significant difference in total neutrophil counts. Only 3 of the 36 patients with documented bacterial infection in the >20% smudge cell group had a neutrophils >8.5 x109/L. Of 13 infants <1yr of age with >20%smudge cells, 5 had a bacterial infection with normal neutrophil counts.
When the smudge cells were separated according to their category, NETs vs DLs, the DL group was older, had more LPD, higher total WBC, lymphocyte and monocyte counts (p=0.000044, 0.00036, 0.018, 0.022, 0.033) [Table 2]. Slides with mostly NETs had higher LAP scores than those classified as mostly DLs (172 +30.5 vs 103.3 +30.8, p=0.0087).
Conclusions: NETosis is a relatively newly discovered tool in the neutrophil's arsenal. This study is the first to identify NETs on peripheral smear evaluations as performed by a routine Hematology Autoanalyzer and to differentiate them from DLs using a reliable set of morphologic characteristics, immunohistochemical stains, and flow cytometry probes. This study also supports data that associate NETs with bacterial infections. This could be clinically useful in diagnosis of infection in the absence of leukocytosis.
Billett:Albert Einstein College of Medicine: Patents & Royalties: Patent application pending for NETs AI software. Kushnir:Janssen Pharmaceuticals: Research Funding. Reyes Gil:Albert Einstein College of Medicine: Patents & Royalties: Patent application pending for NETs AI software.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal