Background:
Sickle cell disease is one of the most common inherited red blood cell disorders, yet many are not aware of their carrier status (Treadwell, J Nat Med Assoc, 2006), which can lead to confusion around pregnancy and newborn diagnosis. Furthermore, data is emerging about the severe and life-threatening risks of sickle cell trait (Kark, NEJM, 1987 and Olaniran, Am J Nephro, 2019). The American College of Obstetricians and Gynecologists' guidelines recommend that pregnant women of African, Mediterranean and Southeast Asian descent be screened for hemoglobinopathies with a complete blood count (CBC) and hemoglobin electrophoresis (ACOG, Opinion #691, 2017). However, adherence to this practice and frequency of improper screening with Sickledex is unknown. Proper screening and counseling can impact families' knowledge and allow them to establish relationships with hematology providers earlier.
Objectives:
We sought to assess prenatal hemoglobinopathy screening practice patterns and methods of Obstetrics & Gynecology (OBGYN) and Family Medicine (FM) providers in the Tri-State regional area.
Methods:
A cross-sectional electronic survey was administered to OBGYN and FM practitioners from six tri-state area institutions using publicly available information and contacts at each institution. Questions focused on prenatal hemoglobinopathy screening practices using case scenarios with variations on parental trait status and ethnicities. Chi-square analyses were used to compare the two provider groups on categorical variables.
Results:
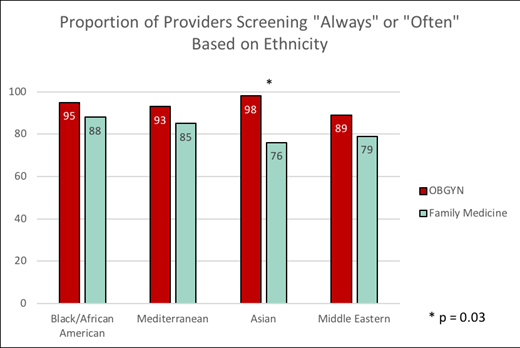
There were 167 total responses; 120 surveys were complete, of which 87 were OBGYN and 33 FM providers. Respondents were mainly faculty (69/120, 58%) and from academic medical centers (n=107). 42% of providers reported that they ask "76-100%" of their patients about a personal history of sickle cell disease or trait. When asked about the proportion of pregnant patients with a positive family history of a hemoglobinopathy, there was a significant difference between OBGYN and FM providers, with 95% of OBGYN providers responding that they screen "76-100%" of those patients as opposed to only 75% of FM providers screening with the same frequency (p=0.0034). When asked about screening practices for patients without a personal/family history of a hemoglobinopathy, OBGYN providers consistently screen more frequently (Figure 1). When analyzed by ethnic background, screening practices were significantly different only between the subspecialty providers who "always" or "often" screened for hemoglobinopathies in mothers of Asian descent (p=0.03). Over 73% of providers report that they "always" screen patients of Mediterranean, Asian, and Middle Eastern descent and 84% always screen patients of Black descent. Over 30% of all respondents said they would use Sickledex for screening in case scenarios for a Black/African American mother, even when it was already known that she is a sickle cell carrier. In cases where the mother's hemoglobinopathy status was unknown, over 80% of providers responded that they would "always" evaluate with a hemoglobin electrophoresis regardless of Black/African American or Mediterranean descent. In terms of referrals to Hematology, in a case where both parents have sickle cell trait 46% of providers would "never" refer that family to Hematology.
Conclusion:
This pilot survey highlights differences in the methods and likelihood of prenatal hemoglobinopathy screening based on the type of prenatal care provider. Screening differences can lead to variations in prenatal guidance, diagnostic procedures, informed decision-making and knowledge of families referred to pediatric hematology clinics. This is the first study analyzing prenatal screening for hemoglobinopathies in OBGYN and FM. This study demonstrates that not all prenatal providers adhere to existing ACOG recommendations regarding which patients to screen for hemoglobinopathies and suggests an actionable area in which to enhance education for prenatal providers. Specifically, providers need to be educated that the use of Sickledex is an inappropriate laboratory screening test, since it will not detect other hemoglobinopathies. Improving prenatal screening practices by collaborating with hematologists may increase adherence to guidelines and allow for earlier relationship building with hematology.
Manwani:GBT: Consultancy, Research Funding; Novartis: Consultancy; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal