Background
In 2017, the US Food and Drug Administration (FDA) approved Endari (L-glutamine oral powder) for patients age five years and older with sickle cell disease (SCD) to reduce sickle cell-related acute pain events and hospitalizations1. This was applauded as the first medication approval for SCD in almost 20 years, following Hydroxyurea (HU) in 1998. We report our experience with barriers to accessibility to a new medication such as Endari, and patients' adherence in adults with SCD in an urban adult sickle cell center.
Methods
After prospectively establishing internal guidelines for the use of Endari, adult patients with SCD seen in clinic at a large urban adult SCD center were prescribed Endari via a local specialty pharmacy, over a 14 month period. Upon return to clinic, patients were asked about barriers to obtaining the medication and adherence to the twice a day dosing. Adherence was also evaluated by calculating the mean possession ratio (MPR) utilizing pharmacy records.
Results
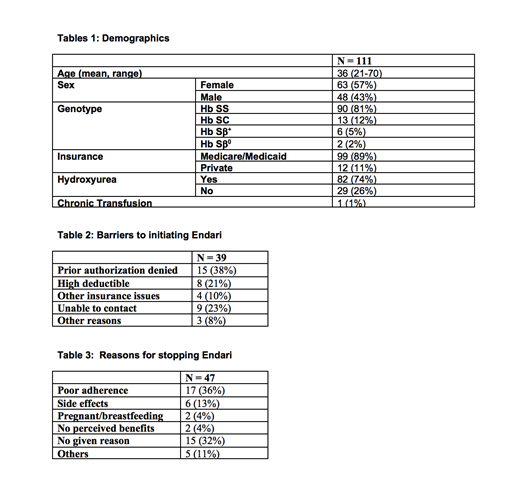
111 patients with SCD (57% females) were prescribed Endari over a 14 month period (Table 1): 83% with severe disease genotypes (Hb SS/Sβ0), 17% with "milder" genotypes (Hb SC/Sβ+). Mean age was 36 years old. 74% of patients were on concomitant HU and 1% on chronic transfusions (>6 months). At the end of the 14 month period, 21 patients (19%) were actively taking Endari, 47 (42%) had discontinued it, 39 (35%) never filled the prescription, and 4 (4%) had received but never initiated therapy. Of the 39 who never filled the initial prescription, barriers included denial of prior authorizations (38% of patients), high deductibles (21%), and inability of pharmacy to contact patient after approval was obtained (23%) (Table 2). Reasons for discontinuing Endari included poor adherence (36%), as defined by patients who did not refill after the initial/subsequent prescriptions (mean refill 1.79 times) and/or missed follow up appointments, side effects (13%), no perceived benefit (4%), and pregnancy/breastfeeding (4%) (Table 3). Average MPR for the 21 patients that are still taking Endari is 0.73, similar to the adherence reported in the landmark phase III trial (77.4%)1.
Discussion
This is the first study that addresses both acceptance of a new medication by the sickle cell population and the barriers to obtaining it. We identified significant barriers to the initiation of Endari in our urban adult SCD patient population and a high rate of self-discontinuation. Patients who discontinued Endari, did so after a median of 47 days after the initial prescription.
The most common reasons for not initiating therapy, present in ~ 70% of the cases, were insurance-related issues, such as prior authorization denial or high deductible/co-pays. In 30% of the cases patients were not reachable or had other issues for not filling it, despite obtaining prior authorization, which may indicate a lack of interest on their part. A small number of patients (6) reported discontinuing due to side effects. After 14 months, only 21/111, ~20% of the original cohort of patients prescribed Endari, reported taking it. The MPR of the patients that were taking the medication was 0.73, similar to the adherence in the Endari study (77.4%)1. Prospective studies are needed to confirm if this pattern is reproducible in other patients' populations across the country and to investigate whether the introduction of a new drug affects adherence to HU.
As experienced with HU, several years elapsed from initial FDA approval to its being more accepted and widely used, and adherence remains sub-optimal. From our report, it is critical to evaluate and mitigate barriers to initiation and adherence to Endari, to ensure it is available to and accepted by the patient population it gained approval and was intended for.
1. N Engl J Med.2018 Jul 19;379(3):226-235
Ogu:Vertex Pharmaceuticals: Consultancy. Minniti:Doris Duke Foundation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal