INTRODUCTION
Sickle cell disease (SCD) is characterized by episodes of painful vaso-occlusive crises (VOC) and progressive end-organ damage, resulting in poor quality of life and a shortened lifespan. Activated and aged neutrophils are pivotal in pathogenesis of VOC. SCD patients exhibit pathophysiologic changes in the intestine. We previously reported intestinal dysbiosis (Lim et al, Am J Hematol, 2016), and increased intestinal injury and bacterial translocation in SCD patients (Dutta et al, J Transl Med, 2019). These patients also exhibited elevated levels of activated and circulating aged neutrophils (CANs) (Dutta et al, J Transl Med, 2019). Since rifaximin is minimally absorbed into the systemic circulation, we sought to determine how the local effects of rifaximin affects intestinal pathophysiologic changes and circulating neutrophils in SCD patients. We investigated these changes in a cohort of SCD patients accrued to a Phase 2 study of rifaximin for SCD (Clinicaltrials.gov: NCT03719729).
METHODS
Twelve SCD patients (5 males, 7 females) with a median age 29 years (range 23-56) received 550 mg rifaximin twice daily for 6 months. Blood, urine and stool samples were collected from patients in steady state before and at different intervals during rifaximin treatment. Intestinal microbiome was evaluated by 16S rRNA gene sequence analysis. The following fluorophore-conjugated monoclonal antibodies were used to evaluate CANs: Gr-1-FITC, CD115-PE-Cy7, CXCR4-PE and CD62L-APC. Flow cytometry was performed using the Moflo XDP Sorter and neutrophils gated by Gr-1Hi CD115Lo SSCHi, and CANs were gated by CXCR4Hi CD62LLo within the neutrophil population. Propidium iodide, FSC and SSC were used to exclude dead cells. Urinary 3-indoxyl sulfate (3-IS), and serum soluble CD62L, intestinal fatty acid binding protein (iFABP) and lipopolysaccharide (LPS) were evaluated in triplicates by ELISA using commercially available ELISA kits.
RESULTS
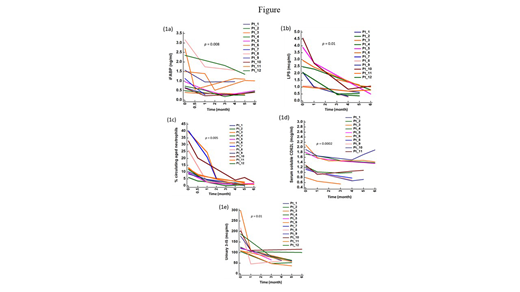
Rifaximin treatment resulted in a decrease in the intestinal injury, as shown by significant drops in the serum iFABP (p = 0.008) (Figure 1a). The improvement in intestinal integrity was observed as early as two weeks into rifaximin therapy. There were also corresponding decreases in the serum LPS levels (p = 0.01) (Figure 1b) and they also occurred as early as two weeks into rifaximin therapy. Both parameters attained levels comparable to those we previously observed in controls who had similar degree of anemia but without SCD.
LPS is one of the pathogen-associated molecular patterns (PAMPs) that trigger toll-like receptors 2/4 (TLRs 2/4) and myeloid differentiation factor 88 (Myd88). Since TLRs2/4 and Myd88 are known to drive neutrophil aging, we next examined changes in CANs. Following rifaximin therapy, CANs decreased significantly in these patients (p = 0.005) (Figure 1c). The decrease was associated with a parallel decline in the number of activated neutrophils, as shown by declines in the serum CD62L (p = 0.0002) (Figure 1d). Unlike CANs, however, the drops in the serum CD62L were not as consistent in some patients and these inconsistencies corresponded with recovery from VOC, highlighting differences in the origins of neutrophil ageing and activation.
Not surprisingly, rifaximin alters the profile of the intestinal metabolomics. Rifaximin also resulted in a decrease in urinary 3-IS (p = 0.01) (Figure 1e), being compatible with a narrowing of the intestinal microbial diversity and suggests a reduction in Clostridiales, the major producers of intestinal short-chain fatty acids such as butyrate.
CONCLUSION
Rifaximin therapy results in improvement in the intestinal pathophysiologic changes observed in SCD. It also reduces the neutrophil subsets pivotal for the pathogenesis of VOC. However, these are achieved in association with a reduction in the intestinal microbial diversity. Further works are needed to delineate the mechanisms rifaximin reduces intestinal injury in SCD.
No relevant conflicts of interest to declare.
Rifaximin for sickle cell disease
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal