Background: Children and adolescents with sickle cell disease (SCD) are at significant risk for cerebral infarction and neurocognitive deficits. In a quantitative meta-analysis, Prussien et al. (2019) showed that school-aged children with SCD display significant deficits in full scale IQ, verbal reasoning, perceptual reasoning, executive function, and processing speed relative to the normative mean in sibling and healthy controls, with mean standard scores ranging from 82.38 to 87.51. Quantitative reviews have also shown that deficits in cognitive function in this population also increase with age (Prussien et al., 2019; Schatz et al., 2002). Few studies have investigated whether therapeutic interventions to prevent cerebral infarction impact progressive neurocognitive benefits in individuals with SCD. Four studies to date have assessed the effect of bone marrow transplantation (BMT) on cognition in SCD, and findings show that full scale IQ remained stable after transplant (Neha Bhatnagar et al, 2011; Bockenmeyer et al., 2013; King et al., 2019; Woodard et al., 2005). King et al., also found that verbal IQ and performance IQ also remain stable. However, these findings are based on very small samples, and replication is necessary across multiple domains of cognition including various transplant approaches. We hypothesize that successful related haploidentical BMT (haplo-BMT) in individuals with SCD will result in stable to improved neurocognitive function.
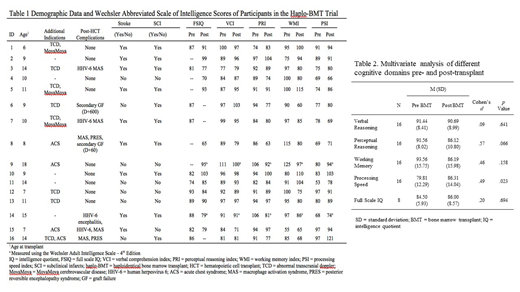
Method: In a select cohort of patients who underwent reduced intensity conditioning haplo-BMT with post-transplant cytoxan for SCD as part of an international learning collaborative. Neurocognitive assessments were conducted 2-3 months prior and 12 months post-transplant. All participants were administered age-appropriate Wechsler scale of intelligence (i.e., Wechsler Intelligence Scale for Children - Fourth Edition for children ages 6 to 16 years and the Wechsler Adult Intelligence Scale - Fourth Edition for adolescents over age 18 years). The transplant data base was used to assess baseline demographics and transplant related outcomes. Descriptive statistics was used to evaluate pre- and post-transplant cognitive function. Only participants who completed both pre- and post-transplant cognitive assessments were included for analysis.
Results: All sixteen patients had sickle cell anemia (Hb SS), and completed both pre- and post-transplant cognitive assessments. Indication for transplant included stroke 56% (9/16), silent infarcts 63% (10/16) and both in 50% (8/16) (Table 1). Results show that despite disease severity, the current sample of adolescents demonstrated greater scores in verbal reasoning, perceptual reasoning, and executive function relative to prior meta-analytic findings for school-aged children (Prussien et al., 2019). Findings from repeated measures t tests (Table 2), showed no significant difference in mean scores pre- and post-transplant in verbal reasoning (pre = 91.44, post = 90.69, d = .09, p = .641), perceptual reasoning (pre = 91.56, post = 86.12, d = .57, p = .066), working memory (pre = 93.56, post = 86.19, d = .46, p = .158), and full scale IQ (pre = 84.50, post = 86.00, d = .20, p = .694); however, mean scores for processing speed were significantly greater post-transplant relative to pre-transplant (pre = 79.81, post = 86.31, d = .49, p = .023).
Conclusions: Neurocognitive function outcomes are stable to improved following haplo-BMT with post-transplant cytoxan in children and adolescents with SCD. Future studies should evaluate long-term neurocognitive function outcomes in SCD patients undergoing haplo-BMT compared to age-matched cohorts on best supportive care.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal