
Backgrounds
Chimeric antigen receptor (CAR) T cell therapy targeting CD19 has demonstrated 80-90% complete remission (CR) rate in R/R B-ALL; however, 10% to 20% of patients have no response and the potential etiology and risk factors remain unclear.
Patients and Methods
From Apr. 2017 to Mar. 2019, 254 patients with R/R B-ALL received treatment at our single center with a second-generation CD 19 CAR-T from 5 companies (NCT03173417; ChiCTR-ONC-17012829; NCT02546739; ChiCTR1800016541; and NCT03671460). The targeted median infused CAR-T cell dose was 3x105/kg. For all patients, screening was undertaken for 58 types of B-ALL related gene mutations and 49 congenital immune deficiency gene mutations using next generation sequencing (NGS) method. The patient and CAR-T product characteristics were analyzed to see if any factors affected the initial CR rate. Univariate analysis comparing CR rates between subgroups were carried out using chi-squared tests. Logistic regression model was adopted for multivariate analysis.
Results
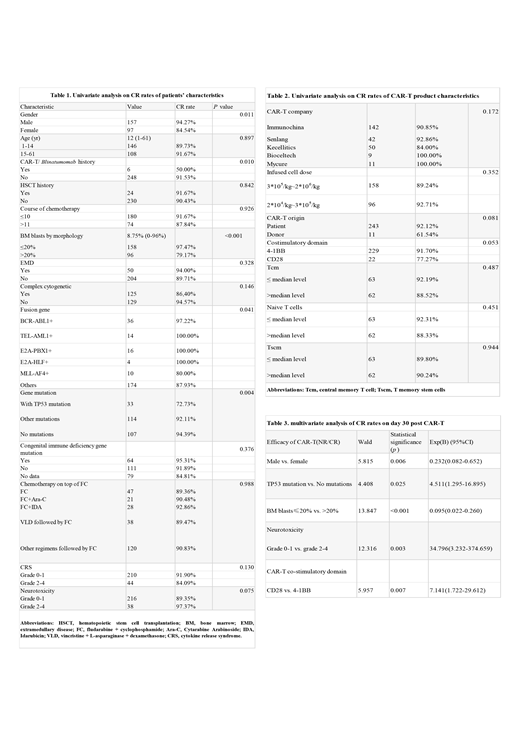
On D30, 90.6% (230/254) patients achieved CR, and minimal residual disease (MRD)-negative CR was 89.4% (227/254). Univariate analysis (Table 1&2) showed a statistical difference in CR rate between females and males (84.54% vs. 94.27%, p=0.011). The CR rate of patients who received prior either CAR-T or blinatumomab treatment was lower than those who had not (50% vs. 91.53%, p=0.01). For the characteristic fusion genes, the CR rate in patients with MLL-AF4 was 80%, which was inferior to those with other or no fusion genes (P=0.041). For gene mutations, a lower CR rate was observed in patients with TP53 mutation compared to those with other or no mutations (72.73% vs. 92.11% vs. 94.39%, P=0.004). Presence of congenital immune deficiency gene mutations did not affect CR rate. Patients with >20% bone marrow (BM) blasts had a worse outcome than those with BM blasts≤20% (79.17% vs. 97.47%, p<0.001). There were no differences in CR between patients age 1-14 yr and >14 yr, patients with or without extramedullary disease (EMD), or patients receiving different chemotherapies between enrollment and CAR-T cells infusion on top of fludarabine and cyclophosphamide (FC) conditioning regimen. Cytokine release syndrome (CRS) and neurotoxicity had no effect on CR rate.There was a trend towards a lower CR rate in patients who received donor-derived CAR-T versus patient-derived CAR-T products (61.54% vs. 92.12%, p = 0.081). A lower CR rate was observed in patients who received CD28 costimulatory domain versus 4-1BB CAR-T products (77.27% vs. 91.70%, p=0.053). There was no difference in CR rate between patients infused with cell dose ≥3x105/kg vs. cell dose <3x105/kg and >2x104/kg. No CR difference was observed from different manufacturing companies. Moreover, 125/254 cases had available data for analysis on subsets of CAR-T cells including central memory T cells (Tcm), naive T cells and T memory stem cells (Tscm). Each group was divided into high- or low-level groups based on the median level. The CR rate was 92.19% vs. 88.52% in high and low Tcm groups, 92.31% vs. 88.33% in high or low naive group, and 89.80% vs.90.24% in high and low Tscm groups, respectively. No difference in CR between the groups were observed.
Multivariate analysis was performed to investigate factors affecting achievement of CR (Table 3). Female group had lower odds of achieving CR after CAR-T therapy compared to male group [OR=0.232(95%CI 0.082-0.652)]. Compared to patients without TP53 mutation or only with other gene mutations, patients with TP53 mutation were more likely to have a low CR rate after CAR-T treatment [OR=4.511(95%CI 1.295-16.895)]. Patients with BM blast >20% had lower odds of achieving CR compared to those with BM blast ≤20% [OR=0.095 (95%CI 0.022-0.260)]. Treatment with CAR-T with CD28 as a costimulatory domain resulted lower odds of CR compared to treatment with CAR-T with 4-1BB [OR=7.141 (95%CI 1.722-29.612)]. Patients who developed severe neurotoxicity (grade 2-4) post CAR-T had higher odds of achieving CR compared to patients with grade 0-1 neurotoxicity [OR=34.796(95%CI 3.232-374.659)].
Conclusions
In this analysis, we have observed that significant risk factors for not achieving CR after CD-19 CAR-T therapy include female gender, BM blasts more than 20%, a positive TP53 mutation, treatment with CD28 co-stimulatory domain vs 4-1BB CAR-T product, and mild as opposed to severe CAR-T related neurotoxicity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal