Introduction: Classical Hodgkin lymphoma (cHL) is highly curable with front-line multi-agent chemotherapy with or without radiotherapy. The treatment landscape is rapidly evolving, with a continued focus on optimizing available therapies in order to improve outcomes and minimize toxicity. Randomized controlled trials provide valuable insights into new treatments and outcomes; however, real-world data describing treatment effectiveness, safety, and health-related quality of life (HRQoL) are limited. This analysis was conducted to understand patient-reported outcomes (PROs) in patients who were treated for newly diagnosed cHL across a range of academic and community settings.
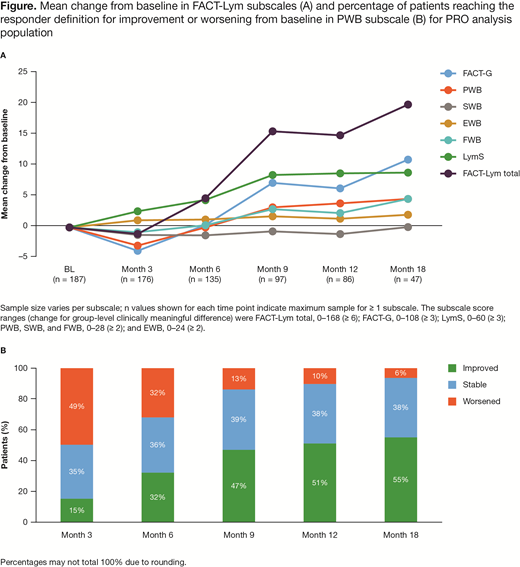
Methods: Study CA209655 is an ongoing, prospective, observational study (NCT02856646) at ~80 US oncology practices with a target enrollment of 500 patients and a planned follow-up of ≤ 5 years. Eligible patients are ≥ 18 years old with histologically confirmed cHL and are treatment naive or within ± 2 weeks of beginning any line of therapy at time of enrollment. HRQoL is a secondary endpoint and evaluated using the Functional Assessment of Cancer Therapy-Lymphoma (FACT-Lym) questionnaire. The FACT-Lym combines a generic cancer-related core consisting of the FACT-General (FACT-G; 27 items) that assesses physical (PWB; 7 items), social/family (SWB; 7 items), emotional (EWB; 6 items), and functional well-being (FWB; 7 items), and a 15-item disease-specific lymphoma subscale (LymS) that assesses lymphoma-specific symptoms. PROs were assessed using questionnaires at baseline (BL), every 3-6 months for ≤ 2 years, and annually thereafter. All patients with BL and ≥ 1 post-BL assessment were included in the PRO analysis. Completion rates and changes from BL scores were evaluated descriptively and analyzed based on published estimates for clinically important differences and individual responder definitions (Hlubocky et al. Lymphoma 2013; Carter et al. Blood 2008; Yost and Eton. Eval Health Prof 2005). High scores indicate better health/functioning for all scales/subscales.
Results: Of 278 enrolled patients at data cutoff (Feb 2019), 226 (81%) were treatment naive; for those, the most common index therapy was chemotherapy (n = 210; 93%). The most common index chemotherapies were ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine; n = 187, 83%) and AAVD (adriamycin, brentuximab, vinblastine, dacarbazine; n = 10, 5%). Only patients receiving index chemotherapy were included in the full analysis set. In all, 89% (87/210) of patients had BL and ≥ 1 post-BL assessment and were included in the PRO analysis. PRO completion rate at BL was 97% (204/210) and remained > 70% up to 24 months for the expected population. Analysis of PROs was not feasible after 24 months owing to small patient numbers (≤ 10); therefore, PRO analyses were focused on the first 18 months. At BL, mean (SD) scores were: FACT-Lym total, 122 (24); FACT-G, 82 (15); PWB, 21 (6); SWB, 25 (3); EWB, 18 (4); FWB, 18 (6); and LymS, 40 (11). At 3 months there was a deterioration in mean scores from baseline in FACT-G (−3.8) and PWB (−3.0) (Figure A). Clinically meaningful improvement of mean scores was observed starting at 6 months in LymS (+4.4) and at 9 months in FACT-G (+7.1), PWB (+3.1), FWB (+2.8), and FACT-Lym total (+15.6). There were no clinically meaningful improvements in SWB and EWB. Based on individual responder definitions, ≥ 50% of patients had improvements in PWB (Figure B) and FACT-G from 12 months, and FACT-Lym total from 9 months.
Conclusions: Initial data from this observational study suggest most patients receive multi-agent cytotoxic chemotherapy as first-line treatment of cHL. Patient-reported PWB initially declined with chemotherapy, but improved with time, and patients had a clinically meaningful improvement in HRQoL by 9 months. The timing of this improvement may be due to discontinuation of chemotherapy due to disease control. Future analyses will evaluate the relationship between improvements in HRQoL and other factors including response, use of immunotherapies versus chemotherapy, and the timing of treatment discontinuation.
Study support: Bristol-Myers Squibb.
Svoboda:Seattle Genetics: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Merck: Research Funding; Incyte: Research Funding; Pharmacyclics: Consultancy, Research Funding; AstraZeneca: Consultancy; Celgene: Research Funding; Kyowa: Consultancy; Kite: Consultancy. Armand:Roche: Research Funding; Merck: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Bristol-Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Adaptive: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Affimed: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Otsuka: Research Funding; Sigma Tau: Research Funding; Infinity: Consultancy; Genentech: Research Funding; Pfizer: Consultancy; ADC Therapeutics: Consultancy; Tensha: Research Funding. Taylor:Adelphi Values: Employment, Other: I am an employee of Adelphi Values, a consulting firm who has received payment from Bristol-Myers Squibb for statistical data analysis in Bristol-Myers Squibb's trials. Sun:Adelphi Values: Employment. Gajavelli:Bristol-Myers Squibb: Employment. Peterson:Bristol-Myers Squibb: Employment, Equity Ownership. Chen:Bristol-Myers Squibb: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal