Introduction: Myelofibrosis (MF) is a rare bone marrow cancer classified as a myeloproliferative neoplasm in which bone marrow is replaced by fibrous (scar) tissue, impairing the production of normal blood cells. MF has a global incidence of approximately 0.58 new cases per 100,000 person-years, with many patients experiencing short survival (approximately 6 years). Most patients with MF are found to have either intermediate-2 or high-risk MF, as per their prognostic score (International Prognostic Scoring System [IPSS] or Dynamic IPSS). The economic impact of MF has been studied in individual real-world settings, each of which may have limited generalizability; however, the holistic economic burden of MF is not well understood. The objective of this systematic literature review (SLR) was to describe economic evidence for patients with MF including cost and resource use data.
Methods: A SLR was conducted in Embase®, MEDLINE®, the National Health Service Economic Evaluation Database (NHS EED), and the American Economic Association (AEA) EconLit® to identify evidence published from database inception to July 2018. Conference proceedings and bibliographies were also searched. Studies were included if they were published in the English language and reported economic burden associated with adult patients with MF. The evidence was not restricted by any country or time limits. Two reviewers assessed each citation against predefined eligibility criteria, with discrepancies reconciled by a third independent reviewer. All the extracted data were quality checked by a second independent reviewer. A descriptive qualitative analysis was conducted to identify the patterns of economic burden in MF across different countries.
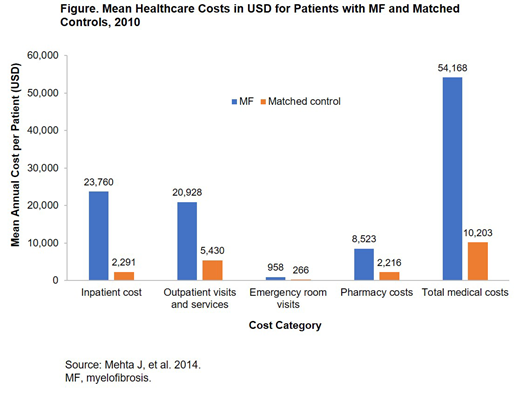
Results: A total of 771 potentially relevant abstracts were identified and screened, of which 23 studies were included in the final analysis. Eleven studies reported cost data only, 10 studies reported both cost and resource use data, and 2 studies reported on the budget impact of treatment for MF. Eight of the included studies were conducted in the USA, 2 each in the UK, Canada, and Ireland, and the remaining 9 reported data from other countries. Eight of the included studies reported total MF costs, 4 studies reported productivity losses related to employment, and 3 studies reported indirect costs related to productivity and informal care. The remaining studies reported cost-effectiveness data for the treatment of MF. Of the 5 studies that reported categorical costs, 3 reported that outpatient costs were the major driver of costs, followed by inpatient costs. Among the studies conducted in the USA, total medical healthcare costs associated with MF ranged from USD 21,000 to USD 66,000 per patient. Three European studies reported that the annual productivity losses per patient ranged from EUR 7,774 to EUR 11,000, with total annual productivity losses as high as EUR 217,975. Two US studies compared the total MF-related healthcare costs with age- and sex-matched controls; costs were significantly higher in the MF cohort compared with matched controls (P < 0.05), especially for inpatient costs, outpatient costs, and pharmacy costs (Figure). Four studies, with a majority of the MF patients aged > 50 years, reported that 20-60% of the patients were absent from work, with a mean of 6.2 hours of work missed in the past 7 days. Among the hospitalized patients, 3 studies reported that the median length of stay for patients with MF ranged from 2.5 to 6.6 days, with 46% of patients utilizing emergency room visits and services.
Conclusions: MF is associated with significant economic burden and work productivity loss to the health system, patients, and their families. Sustained efforts to develop more effective treatments are required in order to reduce the economic burden associated with MF and help patients and physicians improve disease management.
Tang:Celgene Corporation: Employment, Equity Ownership. Taneja:BresMed Health Solutions Ltd: Employment. Rajora:BresMed Health Solutions Ltd: Employment. Patel:BresMed: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal