BACKGROUND:
Financial and regulatory incentives stemming from the Health Information Technology for Economic and Clinic Health Act have encouraged and, hence, increased the availability of online patient portals ('portals') that connect to electronic health records. Through portals, caregivers have direct access to portions of their child's medical record. Direct access is intended to engage caregivers in treatment and, consequently, to improve disease management. However, demonstrated associations between portal use and engagement in care is limited within pediatrics and non-existent in pediatric oncology.
Caregivers of children with cancer have increased anxiety in response to their child's diagnosis and treatment (Myers et al, Cancer, 2014). Allowing caregivers swift access to results via portals may reduce anxiety for some, however, complicated written material may exacerbate anxiety and cause confusion (Schultz, et al, Pediatric Blood & Cancer, 2018). Furthermore, differences in sociodemographic variables between portal users and non-users potentially highlights widening healthcare disparities. Little is known about the use of portals by caregivers of children with cancer or what effect use may have on caregivers. As a first step, this study sought to examine whether sociodemographic and clinical care variables are associated with portal activation in a pediatric oncology sample.
METHODS:
Data were extracted from the electronic health records of pediatric oncology patients diagnosed or treated for their first known cancer within Nemours Center for Cancer and Blood Disorders in the Delaware Valley from January 1, 2012 through June 30, 2017. Sociodemographic variables (patient age, gender, race, preferred language, insurance, zip-code), clinical characteristics (cancer type, date of diagnosis, total number of laboratory and radiology tests within the study period), and portal activation date were gathered. A cost of living index (COLI) was computed using zip-code data. Cancer type was classified as "liquid" or "solid" based on chemotherapy and radiology follow-up procedures. Those who activated the portal more than 30 days before a cancer diagnosis were excluded from evaluation to better isolate portal activation related to cancer diagnosis. Data were summarized with descriptive statistics. Chi-square and independent samples t-tests compared those who did and did not activate the portal.
RESULTS:
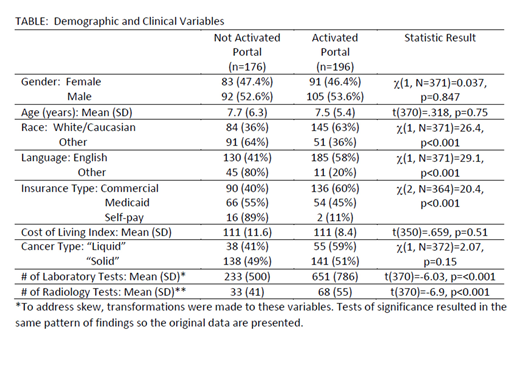
The initial sample included 445 children; 73 families activated the portal more than 30 days before cancer diagnosis. Of the remaining 372 patients, 197 families (53%) activated the portal. Those who activated did not differ from those who did not in regard to patient age, gender, COLI, or type of cancer. Those who were of non-majority race, spoke a language other than English, and did not have private insurance were overrepresented among those who did not activate (TABLE). Families of children undergoing more radiology and lab tests were more likely to activate. For those who activated the portal, 39% did so within 1 month of diagnosis (day -30 to day +30), 13% did so from day +31 to +90, 36% did so from day +91 to +365, and 11% did so greater than 366 days post diagnosis.
CONCLUSION:
There are significant differences in patient portal activation by race, preferred language, and type of insurance. These results suggest sociodemographic disparities in portal activation, similar to patterns found in our pediatric primary care network (Ketterer et al, Academic Pediatrics, 2013). In that sample, however, only 26% of patients activated accounts in contrast to the 53% of families in pediatric oncology activating accounts. In our sample, while general type of cancer was not associated with portal activation, greater burden of treatment evaluation was. This study is the initial step in a program of research evaluating the use, utility, and outcomes of portal use in pediatric oncology. Further work will include evaluation of patterns of portal usage along with evaluations of health literacy and portal related anxiety. As portals become more ubiquitous, we must better understand how they are used and mitigate any disparities in or ill effects of access to this information.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal