Background
Sickle cell disease (SCD) is associated with acute healthcare utilization and an estimated annual cost of $2 billion that is primarily covered through public insurance. Understanding factors contributing to acute healthcare utilization among SCD patients is crucial to decrease costs associated with services. Our study describes trends of acute care utilization among Illinois (IL) residents with SCD over a 3 year period and examines factors associated with hospital admissions from the emergency department (ED).
Methods
We extracted ED visits and hospitalizations associated with an ICD-10 code for SCD from the Illinois Comparative Health Care and Hospital Data Reporting Services, a statewide hospital administrative data source for 154 IL non-federal hospitals. Visits from January 2016 to December 2018 were extracted. Variables of interest included patient sociodemographic variables (age, IL region, insurance, zip code poverty rate and area deprivation index and distance to care). Poverty was categorized based on the percent of residents in a zip code who are at or below the federal poverty level (FPL) as low (<10% of households ≤ FPL), medium (10-20% of households ≤ FPL) or high (>20% households ≤ FPL) using data from the 2017 Community American Survey. Composite socioeconomic opportunity was determined using 2015 state ranked patient zip code area deprivation index (ADI) and categorized as low (ADI<5), medium (ADI=5-7.99), or high (ADI≥8) with higher ADI levels indicating higher levels of socioeconomic disadvantage. For admissions, length of stay (LOS) and intensive care unit (ICU) care were examined. Health care facilities were categorized by number of SCD visits per year into low (< 50), medium (50 to 332) or high (≥333) volume. Poisson regression, adjusted for clustering within hospitals, was used to analyze the likelihood of hospital admission versus discharge from an ED visit.
Results
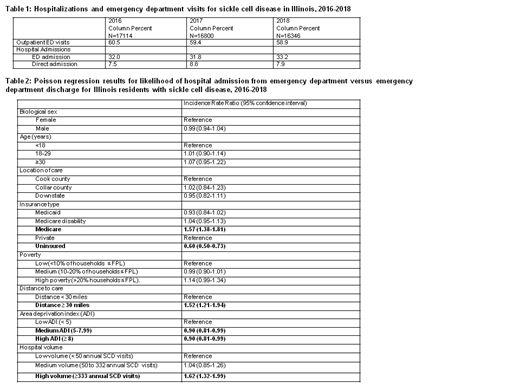
Trends of acute care utilization. There were 50,260 hospitalization and ED visits with SCD codes in the 36 month study period, averaging 1396 visits per month. The number of visits per year was stable during the study period (Table 1). Approximately 71% of the visits were associated with SCD as the primary diagnosis. The majority (64%) of visits occurred in Cook County, with 95% occurring within a 30 miles radius from the patient's zip code and 94% in facilities with more than 50 SCD visits annually. Most visits were covered under public insurance (50% Medicaid and 25% Medicare); 20% were covered by private insurance; and less than 5% were uninsured visits. The majority of visits were from patients living in medium (46%) or high (32%) ADI with only 19% from low ADI zip codes. Most (60%) visits were outpatient ED visits (average 832 visits per month) and 40% were hospital admissions (average 564 visits per months) with a mean LOS of 5 days and 12.8% requiring ICU level care. Approximately 80% of the hospital admissions were admissions from the ED.
Factors associated with hospital admissions from the ED (Table 2). In the adjusted model, uninsured patients were less likely to be admitted (IRR=0.60; 95% CI 0.50-0.73) and Medicare patients were more likely to be admitted (IRR=1.57; 95% CI 1.38-1.81) compared to patients with private insurance. ED visits with patients travelling >30 miles (IRR=1.52, 95% CI 1.21-1.94) and visits at high volume hospitals (IRR=1.62; 95% CI 1.32-1.99) were more likely to result in admission compared to visits associated with shorter distances and visits at lower volume hospitals, respectively. Visits with patients from medium ADI zip codes (IRR=0.90; 95% CI 0.81-0.99) or high ADI zip codes (IRR=0.90; 95% CI 0.81-0.99) were less likely to result in admission than visits from low ADI zip codes. Biological sex, age, location of care, and zip code poverty level were not significantly associated with hospital admissions from the ED.
Conclusions
In the most recent 3 year period, SCD acute healthcare utilization in Illinois remained stable without significant reductions. Patients who were uninsured or had higher levels of socioeconomic disadvantage were less likely to be admitted from the ED whereas further distance to care and high SCD volume hospital were associated with higher rates of admission. Further research should explore whether the uninsured and highly disadvantaged were less likely to be admitted due to disease severity or system level factors such as poor access or poor preventative care.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal