
Introduction: The standard of care for patients with hemophilia A without inhibitors is factor VIII (FVIII) replacement therapy. The availability of non-factor therapy such as emicizumab (Hemlibra®; Genentech, Inc., South San Francisco, CA, USA) is changing the treatment landscape. A model was developed from the perspective of the US healthcare system to compare the cost-effectiveness of recombinant FVIII (rFVIII) products (standard half-life [SHL] and extended half-life [EHL]) versus non-factor therapy emicizumab in the treatment of patients with severe hemophilia A without inhibitors.
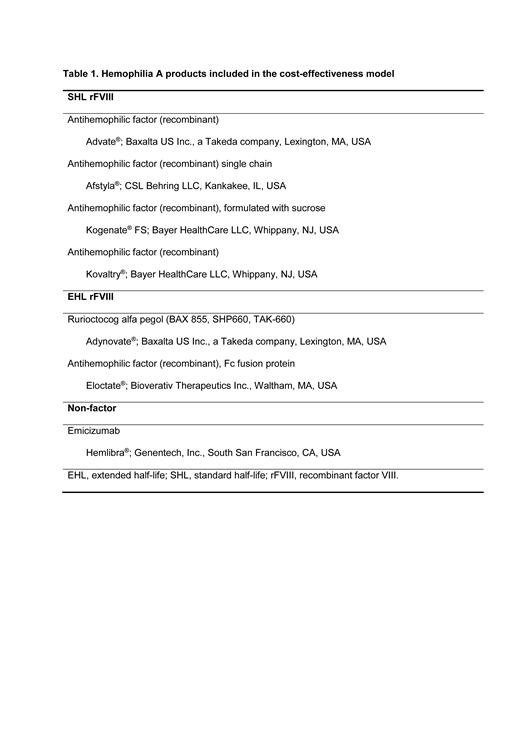
Methods: The Markovian model used in this analysis included 5 mutually exclusive hemophilia A-related health states: with/without target joints (TJs), with/without arthropathy, and death. Health states changed or remained constant, depending on bleeds and recovery probability. Transition to the health state "death" was derived from mortality rates in the general US population according to age. Each health state was associated with costs and utilities that were summed over time. Estimated total costs and treatment effectiveness as measured by quality-adjusted life years (QALYs; a measure of health outcome that incorporates the impact on both quantity and quality of life) for each health state were then used to calculate incremental cost-effectiveness ratios for pairwise comparisons of treatments (prophylaxis or on-demand for a pooled analysis of 6 rFVIII products [SHL and EHL] vs emicizumab prophylaxis; Table 1) over a life-time horizon. Patient data used in the model were based on a systematic literature review and clinical trial results, and network meta-analysis. Model parameters included patient baseline characteristics, change in body weight by age, prior prophylaxis or on-demand treatment, annualized bleeding rate (ABR), probability of developing or resolving TJs or arthropathy, mortality, number infusions per bleed, medical check-ups, and hospitalization. Based on these data, patients in the model were assumed to be male and 33 years of age at baseline; 72.0% had TJs and 58.4% had arthropathy. Probability of developing TJs per joint bleed was estimated to be 0.9% (prophylaxis and on-demand treatment). Probability of developing arthropathy per joint bleed was estimated to be 2.2% for patients who received prior on-demand treatment and patients who received prior prophylaxis were assumed to have no risk of developing arthropathy. The model assumed life-long adherence to the same prophylactic hemophilia treatment. Drug cost was based on 2018 average sales price and dosing was on label. The model did not include treatment-specific adverse events or inhibitor development.
Results: Prophylaxis with rFVIII (SHL and EHL) was estimated to be less costly and more effective (total $13,656,238; QALYs 17.61) versus non-factor prophylaxis with emicizumab (total $16,447,843; QALYs 17.58) over an estimated 70-year lifespan of a patient with severe hemophilia A, which suggests rFVIII prophylaxis is an economically preferable strategy. Total cost consists of costs directly related to prophylactic treatment (rFVIII $12,850,894 vs emicizumab $15,555,379) and costs associated with healthcare resources (rFVIII $805,344 vs emicizumab $892,464). rFVIII prophylaxis was also estimated to be less costly and more effective (total $13,656,238; QALYs 17.61) versus on-demand rFVIII treatment (total $13,823,123; QALYs 12.29).
Conclusions: In this pooled analysis of select SHL and EHL rFVIII products, the results suggest that rFVIII prophylaxis is a cost-effective long-term intervention for patients with severe hemophilia A without inhibitors compared with non-factor prophylaxis with emicizumab and on-demand rFVIII treatment.
Sun:Shire US Inc., a Takeda company: Employment, Other: a Takeda stock owner. Wu:Shire US Inc., a Takeda company: Employment, Other: a Takeda stockowner. McDermott:BresMed Health Solutions Ltd.: Employment. van Keep:BresMed Health Solutions Ltd.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal