Background
Thrombosis is the second leading cause of death for cancer patients undergoing chemotherapy. Despite this, cancer patients also have a higher risk of clinically relevant bleeding related to thrombocytopenia secondary to chemotherapy or underlying disease. Optimal management of venous thromboembolism (VTE) in the setting of these competing risks is difficult. Generally, two strategies are used: (1) full dose anticoagulation with supportive platelet transfusions to maintain platelet count above 40,000-50,000/μL or (2) reduced-dose anticoagulation while platelets are <50,000/μL.
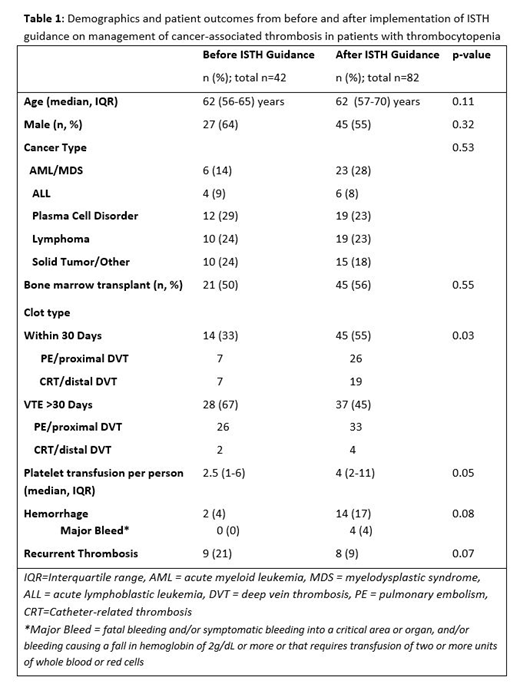
The International Society on Thrombosis and Haemostasis Scientific and Standardization Committee (ISTH SCC) recently released updated guidance on management of anticoagulation in patients with cancer-associated thrombosis (CAT) and thrombocytopenia. We retrospectively reviewed cancer patients diagnosed with VTE and thrombocytopenia before and after implementation of the ISTH SCC guidance to determine the impact of the statement on platelet transfusion, bleeding, and recurrent thrombosis.
Methods
We evaluated cancer patients with thrombocytopenia who required anticoagulation for VTE for 11 months before and after implementation of the ISTH SCC guidance statement. Patients with malignancy, thrombocytopenia (platelets <50,000), and administration of an anticoagulant were identified through an electronic medical search. Charts were retrospectively reviewed to identify the type of VTE event, number of platelet transfusions, incidence of bleeding, and VTE recurrence during thrombocytopenia within the pre- and post-intervention time periods. Cases were excluded if they were treated with anticoagulation for indications other than VTE. Summary statistics were calculated. Chi-square and Fisher's exact tests were used to compare categorical variables. Continuous variables were compared using the Mann-Whitney test.
Results
A total of 42 cases were identified in the pre-intervention time period and 82 cases in the post-intervention time period (Table 1). The median age was 62 years and the majority of patients (55% and 64%) were male. A total of 34 (80%) patients had experienced a PE or proximal DVT in the pre-intervention and 59 (72%) in the post-intervention time period (p=0.27). Significantly less patients experienced a VTE less than 30 days prior to thrombocytopenia in the pre-intervention compared to the post intervention time periods (33% vs. 55%, p=0.03). Likely secondary to this difference in acuity of the thrombosis, there was a trend to an increased per patient platelet transfusion in the post-intervention time period (median 2.5 vs. 4, p=0.05). Hemorrhage was noted in 2 (4%) of cases pre-intervention; and 14 (17%) in the post-intervention, only 4 (4%) of which were considered major hemorrhages by ISTH criteria (fatal bleeding and/or symptomatic bleeding into a critical area or organ, and/or bleeding causing a fall in hemoglobin of 2g/dL or more or that requires transfusion of two or more units of whole blood or red cells). A trend towards less recurrent thrombosis was noted in the post-intervention group (9% vs. 21%, p=0.07). Recurrent VTE events included 2 PE and 15 DVT. Adherence to the guidance statement was excellent (95% for medication management and 98% for platelet transfusions).
Conclusion
The ISTH guidance on management of cancer-associated thrombosis in patients with thrombocytopenia can be successfully implemented in an academic medical center. Trends towards higher incidence of bleeding and reduced incidence of thrombosis occurred.
Baumann Kreuziger:CSL Behring: Consultancy; Vaccine Injury Compensation Program: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal