
Introduction
Platelets are transfused prophylactically to prevent hemorrhage in a variety of patient populations. However, guidelines indicate that prophylactic platelet transfusions in patients with platelet counts above 50k/uL are usually not indicated, with notable exceptions including those undergoing neurological or cardiac bypass surgery. Common minor procedures such as paracentesis, central line placement, and lumbar puncture have been safely performed at platelet counts below 50k/uL. Despite this evidence, our institution incurred approximately 10 million dollars (USD) in direct platelet costs in 2017, with nearly 40% of platelet transfusions are occurring when the patient's platelet count exceeded 50k/uL. Given the significant financial impact of, and potential adverse effects associated with inappropriate platelet transfusion, we implemented a best practice advisory (BPA) in our electronic medical record (EMR) in order to better characterize patterns of platelet transfusion orders in patients with platelet counts >50k/uL.
Methods
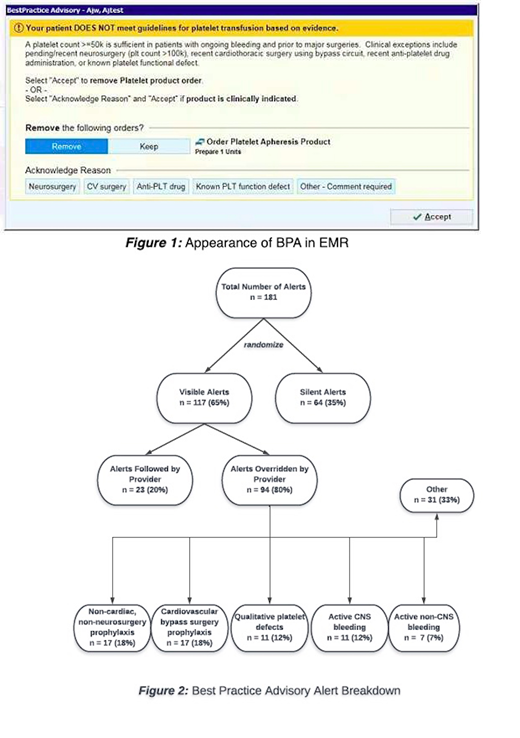
An EMR-embedded BPA was activated in the inpatient hospital setting of a large, tertiary care academic medical center on May 1, 2019, and triggered whenever a platelet transfusion order was placed on an admitted patient whose most recent documented platelet count was >50k/ul. To inform the comparative impact of BPA alerts on provider behavior, alerts were randomized at the patient level to trigger either in standard or silent fashion. For standard alerts, the BPA appeared on-screen, informing the provider that their platelet transfusion order was potentially inappropriate and citing supportive evidence. Providers had the option of following or overriding the alert (Figure 1). In case of alert override, a pre-specified or free text justification was requested. Pre-specified options included upcoming neurosurgery, cardiac bypass surgery, known qualitative platelet defects, or patients taking antiplatelet drugs. Charge data were based on charges for platelet transfusion orders as listed in the hospital charge master.
Results
From May 1, 2019 to July 30, 2019, the alert fired 181 times (Figure 2). Alerts were silently triggered in 64 (35%) cases. Of the 117 active alerts, 23 (20%) were followed and 94 (80%) were overridden. The most common reasons for alert override included prophylactic transfusions ahead of non-cardiac and non-neurosurgical operations (18%), upcoming cardiac bypass surgery (18%), qualitative platelet defects (12%), active central nervous system (CNS) bleeding (12%), and active non-CNS bleeding (7%). The estimated cost savings associated with followed alerts was $18,170 USD.
Discussion
Our BPA was effective in reducing instances of platelet transfusion orders by 20% over a three-month period, translating to an estimated annual savings of nearly $70,000 USD in hospital charges. Conversely, the 80% alert override rate indicates that platelet transfusion in patients with platelet counts >50k/uL remains common, occurring in a variety of contexts. Potentially appropriate reasons for platelet transfusions included orders in the setting of cardiovascular bypass surgery, active CNS bleeding, or qualitative platelet defects, representing circumstances in which platelet thresholds are often set higher than 50k/uL. Alternatively, 25% of alert overrides occurred in potentially inappropriate contexts, including patients undergoing non-cardiovascular/non-neurosurgical procedures and patients with non-CNS active bleeding, settings where routinely targeting a platelet threshold >50k/uL is not supported by evidence.
As a result of our study's randomized design, future directions include comparative analyses between patient care encounters in which alerts were silently versus visibly triggered, allowing for rigorous determination as to whether providers' interaction with our BPA influences subsequent rates of potentially inappropriate platelet utilization as compared to a control group.
Overall, our findings show that platelets are frequently ordered in potentially inappropriate settings, and that reducing these orders imparts significant financial savings. These results provide an impetus for interventions directed at educating providers on appropriate platelet ordering practices, in order to further reduce unnecessary expenditures and optimize patient care.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal